7-12 months
In a normally sighted infant, visual and motor activities increase by the beginning of the second half of the first year. The infant's eyes 'are everywhere' and so are the hands that have a nearly compulsive desire to grasp everything within reach. The infant notices tiny crumbs on the floor and starts to develop pincer grasp to pick them. This activity can be used to measure detection acuity at home during therapy or play: When the infant sits on the floor, a few small sweets are placed behind his back. When the infant is turned on his/her stomach and placed so that the sweets are close to his eyes, the infant supports himself on his arms and -if he notices the sweets- usually stops moving for a moment, looks at the sweets, supports himself on one arm and reaches the other hand toward the sweets to pick them.
A visually impaired child may not yet be able to support himself on one arm and visually impaired children with motor problems also need a modification of the test situation. Infants who can sit in a high chair, can be tested by placing the sweets on the table. If the infant does not yet sit but stands supported, the sweets can be placed on the tray of the supporting stand. Placing the sweets is done either before the infant is brought to the place or as a game: Have a few sweets in both hands, tell the child that something will appear on the table/tray while moving both hands above the table. Now and then drop a sweet from your hand without stopping the movement. When you have dropped a few sweets the infant may spontaneously pick them. If not, search together with the infant what might be on the table.
If the sweets cannot be noticed, try larger sweets, cereals (Cheerios and Rice Crispies are particularly good). Notice that contrast between the colour of the sweets and the surface of the table is an important factor. It is better to use dark small objects on lighter coloured surface than vice versa. Small white objects on dark surface may give a wrong idea of visual acuity. If the child has uncorrected refractive error or cannot accommodate, the blurred image of a small white object may be quite a large blurred ring and thus much more easily noticeable than the object is when seen clearly.
Vision can be assed using grating acuity tests as before and now also with the Cardiff test. Contrast sensitivity is assessed with Hiding Heidi and visual field by confrontation. If visual field defects are noticed, training of use of the less functioning side is started immediately by making the infant aware of objects on that side and by moving interesting things from the better functioning side to the less functioning side. In some cases the measured difference in the use of field halves is not due to visual field loss but loss of attention. With training it often disappears or at least decreases in a few months.
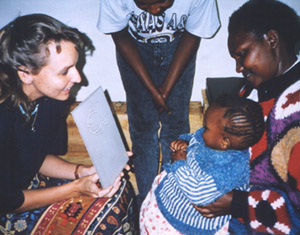
|
Cardiff Card used in assessment of an infant in Kenya. The cards require good care because of their delicate surface. |
Monocular detection acuities can be observed after the child has become accustomed to tolerate covering of one eye by a cap or scarf. Pirate's patch does not work at this age.
Covering an eye is an unpopular thing at this age. If it is done by pushing the infant's cap over one eye when dressing him, it may not be noticed by the infant if the uncovered eye has useful vision that is not much worse than that of the covered eye. By covering the eyes in turn now and then, development of use of vision of both eyes can be followed at home or during therapies. |

|
Development of spatial concepts uses combination of visual information with 'measurements' with the child's own body. To help a visually impaired infant to use visual information in creating spatial concepts, we can use small spaces with clear visual and tactile details. In Nordic countries we call them 'little rooms', a name given by Lilli Nielsen, although small boxes have been used as plaything long before she developed her special little rooms for blind children. For children who have useful vision the little room needs to have accentuated visual structure. That is possible by cutting narrow slits close to the upper edge of a regular brown box.
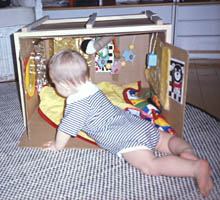
|
A simple brown box can be modified to an effective training tool for orientation in space. The slits close to the upper edge give the infant visual structure of the space. The decorations on the walls have both visual and tactile contrasts to be studied with hands and feet. If the box needs to be moved, a wooden frame makes carrying easier - even with the infant inside. |

|
The toys and other interesting objects hanging from the rubber band are useful in learning the concept of object permanence. The rubber band allows bringing the objects into mouth for exploration and is far enough from the infants face not to hurt him. |

|

|
The box used for training of spatial awareness can be as shabby as this box and yet function well. The infant who was thought to be blind, immediately became an active user of vision and enjoyed glistening toys, was much interested in having his hands in the midline and exploring his feet with his hands.
Visual impairment makes some motor skills more difficult to learn and therefore training of basic motor skills should be started as soon as the infant can start physiotherapy, later specific mobility training for safe moving as soon as the child starts to walk. As seen in the photographs, training of saving responses and balance requires concentration.
Saving responses can be trained like this, on the floor but also when the infant sits on lap by lifting one knee in turn a bit higher thus tilting the infant.

Our balance is usually dependent on the function of our inner ear, information from the peripheral visual field and on proprioseptive information from the lower extremities and trunk. An infant who is learning to sit unsupported does not yet get much information from proprioseption and if peripheral visual field does not function well, balance depends on the function of the inner ear. In such a situation saving reactions require a lot of training.
Moving is often a frustrating effort at the age of 6-7 months when the strength of the arms and legs does not yet carry the weight of the body. Training in water, baby swimming or playing in bathtub develops motor functions, also oculomotor functions.

|
Both healthy and impaired infants benefit from swimming. It gives them freedom to move and develops motor functions and balance. Infants with ear and other infections cannot participate in this fun training. |

