Vision for communication
Visual function at low contrast levels needs to be assessed early, because visual communication is so important in the life of infants and young children. "Hiding Heidi" low contrast game can be used starting from the age of 2-3 months to measure the distances where the infant responds to facial features at different contrast levels. The same test can be used at any age.
In Nordic countries, deaf children use either sign language or lip reading supported by finger spelling or they use both techniques. There are still many places where deaf children are not allowed to use sign language and parents are not taught to sign, so the little infant has to try to understand lipreading without hearing the words. (Try yourself to communicate with someone using only lipreading, or watch the TV without sound and you get an idea how much you loose, even when you know the language.)
Communicative information is visual information in motion, therefore it is important to measure motion perception but presently there are still only experimental tests. RP may affect motion discrimination quite early, on the other hand motion perception seems to be present in ring scotomas that do not respond to the brightest Goldman stimuli (more about the visual field on the next few pages). How much motion perception can be changed without affecting lip reading or finger spelling, is not known. If a youngster complains that seeing finger spelling has become more difficult, changes in motion perception should be kept in mind, and signing modified for optimal clarity.
In good collaboration with all persons involved it is possible to learn to understand even multi-impaired children's communication - after repeated assessments.
Visual communication is usually undisturbed in most RP children through the primary or grade school. Problems occur in high school, college or in young adulthood. Many Usher people have a useful person-to-person communication field until their forties, sometimes to retirement age. Group communication may be disturbed in the teens by the advancing ring scotoma.

Results of Goldmann-perimetry at different ages. First there is a decrease in the size of the isopters I/4 and III/4 (the smallest and the second smallest circle in Figure A) and there are small patches of decreased sensitivity (hatched areas).

Later there is further loss of function in the midperiphery of the visual field, the ring scotoma develops, and becomes absolute (B). An absolute scotoma is an area where there is no response to the largest, brightest light stimulus of the perimeter.

The ring scotoma becomes larger with time until there is only a tubular visual field in the middle and a small peripheral crescent of perception remaining (C).
The size of the visual field can be assessed starting in early infancy using Sheridan's balls, but this test does not reveal changes related to retinitis pigmentosa. The early changes are in the "midperiphery" of the visual field (not in the middle, not at the periphery but in a circular area surrounding the central visual field of approximately 50-60 degrees in diameter). The small patches of diminished function are difficult to measure before the age of 41/2 - 5 years. If a child is given the opportunity to watch Goldmann field testing of an older child, it is easier to teach him/her to keep looking at the fixation target straight ahead and to respond to peripheral stimuli.
 The test situation can be trained by using a flickering light stimulus on a long wand. This technique is also useful in demonstrating scotomas. Place the light, when turned off, within a scotoma that you have measured in perimetry, turn the flicker on and move the light into the functioning part of the visual field to demonstrate the small scotomas the child is unaware of. It is important to explain that everyone of us has similar small scotomas, the blind spot in each eye, and we are not aware of it. In the assessment of a deaf child's visual field using the flickering diode on the wand, it is best to use an interpreter as the fixation target, since communication is then uninterrupted.
The test situation can be trained by using a flickering light stimulus on a long wand. This technique is also useful in demonstrating scotomas. Place the light, when turned off, within a scotoma that you have measured in perimetry, turn the flicker on and move the light into the functioning part of the visual field to demonstrate the small scotomas the child is unaware of. It is important to explain that everyone of us has similar small scotomas, the blind spot in each eye, and we are not aware of it. In the assessment of a deaf child's visual field using the flickering diode on the wand, it is best to use an interpreter as the fixation target, since communication is then uninterrupted.
Goldmann perimetry requires good co-operation from a hearing adult patient. It is a very demanding task to try to measure the visual fields of a five or six year old deaf or hearing child. The instrument is first introduced on both sides, so the child can look through the peep hole and see the eye of the parent or the nurse. The child can also see how the light is moved by the tester (see Deafblindness: Visual Field). The parents can be tested briefly to demonstrate difficulties in responding correctly. After that they appreciate the performance of their child much more and also understand the test results better.
The interpreter for a deaf child in this test situation must be either one with experience in visual field testing and communication with young deaf children in general or sometimes the child's own teacher, if an interpreter is not available. In the latter case it is often necessary to briefly measure the visual field of the teacher as an introduction, otherwise interpretation may not be exact. Parents should not function as interpreters during such a difficult test.
Since no visual communication is possible after the deaf child puts his/her chin on the headrest, I usually tell the child that I will tap him/her on the knee in case fixation is not on the fixation target. This helps the child to hold fixation stable. The hearing child is told to look at the fixation target whenever the eye is noticed to shift fixation. The first examination is more like training than a test. During the second measurement at least one visual field is measured reliably and during the third examination the other. There is a tendency of the largest isopters to move slightly outward between the age of 5 and 9 years after which they may remain stable for some years. This "improvement" is not real but is a sign of improved co-operation.
The time available for Goldmann perimetry is limited. As soon as the child gets bored, the thresholds start to vary. Therefore, it is wise to limit the test to the isopters IV/4 and I/4. If the distance between these two isopters is larger than normal, there is loss of function in the midperipheral field. Loss of sensitivity in the midperiphery may lead to problems in perception of motion, thus ball games may become difficult, but not in all children with RP. One of our best young goal keepers has good size ring scotoma.

Demonstration of the ring scotoma by a youngster makes it easier to understand recordings of Goldmann visual fields. When the child/youngster tells (Video) that he sees his finger movements at the level just in front of his ears, that they look different in midperiphery and that they are again better visible in the centre of the visual field, we remember the structure of his visual field much better than we can remember laboratory results. - It is advisable to ask the youngsters to describe their visual fields as observation of finger movements at several different luminance levels to learn about the effect of changes in illumination. Goldmann visual fields are measured at 10 cd/m2 (candelas per square meter), which is at the border between photopic and mesopic luminance. This level was chosen because it is suitable to early detection of glaucomatous changes, not to evaluate visual functioning. All clinical tests, except finger perimetry, are performed at low luminance levels that overestimate visual field losses in most diffuse retinal degenerations.
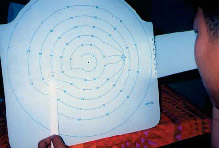

Damato campimetry allows measurement of central visual field in places where the expensive Goldman perimetry is not available. With Damato campimetry we can measure the central visual field and the inner edge of the ring scotoma when it starts to develop.
Damato campimetry can be used from the age of about 5 years. Since few children at that age know numbers well enough to locate the numbers used for fixation of gaze, a pointer with a ring at its end is placed on the number to help the child to hold the fixation on the number. It is wise to start the measurement with a few points in the middle and then measure the blind spot. If this can be documented other small scotomas can also be detected.
 The size of the visual field can be measured by using the confrontation technique, which means that the tester brings his/her hand from behind the person forwards simultaneously moving his/her fingers or uses a white ball or a white dot on grey background as the stimulus. The location in space where the person notices stimulus is recorded.
The size of the visual field can be measured by using the confrontation technique, which means that the tester brings his/her hand from behind the person forwards simultaneously moving his/her fingers or uses a white ball or a white dot on grey background as the stimulus. The location in space where the person notices stimulus is recorded.
When the retinal changes increase in the midperiphery, the patches of loss of vision become confluent and form a ring around central vision. A relative ring scotoma may become absolute at low luminance levels, i.e., the visual field suddenly shrinks when the child enters a dark place. Presently, we do not use standardised techniques for measurement of scotopic visual field except at a few university clinics, although Goldmann perimeters have the facility of measurement at lower luminance levels. If the child seems to have problems following instructions in dim light, confrontation field can and should be measured at low mesopic luminance levels.
In assessment of visual fields, and all other visual functions in RP-children, we should remember to consider how exposed to light the child was before the measurement. If the child comes for the examination on a bright sunny day, visual acuity and contrast sensitivity may be worse than on a cloudy day; and in the visual fields the change is often even more marked.
Measurement of visual field with a Goldmann perimeter is a part of the clinical examination, for which the teacher or therapist can train the child beforehand. The communication field of a youngster whose visual field has decreased to a tubular field, is a test that each teacher and therapist at the school for the deaf and in the integrated education should be able to measure. It is measured in the following way:
- use the usual communication distance of 1.5 -2 meters,
- ask the child to keep looking at your face ("nose") and
- to tell you when he/she notices your hand approaching from the side.
Start with bringing your outreached hand toward your body until the child notices it. Touch your shoulder at this point to give yourself a tactile reference for signing, if you communicate with a deaf child. Then bring your hand from the other side, from above and from below to measure the area in space within which your hands are visible at that particular distance. This space is the child's
At a greater distance his/her communication field is larger. When you get closer, the communication field becomes smaller.
Communication field of a person with tubular visual field becomes larger when the person communicating is at a greater distance. Since the visibility of details decreases at a greater distance, the optimal communication distance is a balance between the size of the communication field and seeing details. Modified from Hyvärinen L, Gimble L, Sorri M, Assessment of Vision and Hearing of Deaf-Blind Persons. Royal Victorian Institute for the Blind, Burwood Educational Series, Burwood 1990.
Each deaf youngster should be able to tell interpreters at which distance the interpreter needs to stand and which size of signing field is comfortable at that distance. If adult persons, teachers, therapists and parents remember to ask the child where they should stand when signing, the child becomes accustomed to expect proper signing during interpreting.
There is a special communication need of deaf children that is poorly understood in many countries: the need to effectively train written language at an early age. We need to start supportive measures in language development when they are effective. In the late forties, if vision impairment prevents use of sign language in communication, the person may not be able to learn written language that is necessary for reading Braille.
Previous Chapter 
|
 Next Chapter Next Chapter
|