Training for testing of visual acuity
It is possible to start measuring recognition visual acuity values much earlier than we usually do by playing the test situation (see: Testing vision of a 23 months old child) with the child as a part of the activities of an early intervention program, kindergarten, a school or at home. In the test situations the child uses either matching or naming so these important functions need to be trained. However, we should be aware of that matching uses purely visual functions and the concept ”same”, whereas using names adds into the testing of vision also language and speech at two different levels: 1) using names of concrete objects: ball/ ring/ hula-hoop; window/ brick/TV; apple/berry/bunny ears/ slippers; house/ dog house/ tent or 2) using much more difficult abstract names: square, circle, fruit, arrow/ mouse (“on the computer screen”).
The play situation varies a lot depending on the spoken or sign language used to communicate with the child or adult with special needs. Therefore our language should be at the level of the child/adult and should not require them to function in the difficult situation at threshold values more than necessary. We do not say “Try to look at these really small pictures”. During training use matching.
Developing the concepts same and different
The LEA Puzzle was designed for 1) easy matching of basic colours and 2) matching of the forms that are used as the optotypes in the visual acuity tests. We learn to match colours before we learn to match forms. While playing with the puzzle pieces of the LEA Puzzle and matching their colours with the colours of the correct cut-outs, the child is also exposed to playing with forms. During this play you have an opportunity to observe eye-hand coordination and visual and motor memory of the location of the cut-outs if the board is rotated 90 or 180 degrees. (The child may turn the puzzle board back to its usual orientation.) Later you also learn which strategy the child uses to rotate the “house” and the “apple” into correct orientation if these puzzle pieces are placed on the board rotated 90 degrees.
As an introduction, the child can watch another child playing with the puzzle or you take the puzzle pieces out of their cut-outs saying “I place these two puzzle pieces on the table (circle and square); now you can place them back on the puzzle board” and the child places the puzzle pieces back one by one. If the child is very young, you may need to let him watch your activity on several days until the child shows interest to put the puzzle pieces in their cut-outs instead of making noises with them. Wait patiently and, if possible; let the child see an older child to play with the puzzle. Do not ask your child to watch what the other child does. He/she will watch when he/she is ready.

Figure 1.
Figure 1. The puzzle is introduced to the child. The girl in these pictures has started to train for testing a few weeks earlier when she got her +6 spectacles for the first time. In such a situation it is important to learn whether the visual acuity values of the eyes are equal or has one of the eyes started to lose its resolving power, is on the way of becoming a ‘lazy eye’. Pictures of this child are frames from videos at Testing Vision of a child with Down syndrome.
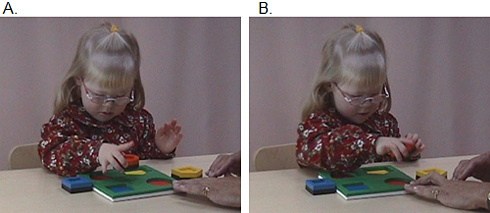
Figure 2.
Figure 2 A & B. To start, the easiest of the forms, the circle is placed in the middle of the puzzle board and the infant/ child is encouraged to find where it can be put. When the child has placed a puzzle piece in its cut-out, respond with a positive calm remark confirming that “the piece got into its own place, the colour of the cut-out is the same as that of the puzzle piece” (no clapping of hands). Then place the round puzzle piece on the table and give the next piece, the square.
In the beginning the puzzle pieces “house” and “apple” are first placed in the middle of the puzzle board in the same orientation as their cut-outs. When the child has played with the Puzzle, you can place the puzzle pieces in a wrong orientation and watch what strategy the child uses to place the puzzle piece in its cut-out. Is it with force or trying different orientations, randomly or with an obvious plan. The hand movements may be difficult to copy so sometimes it is fair to give the child a model of the motor functions when placing the puzzle pieces in the box by saying “when I place this “apple”- or “house”-piece I have to slowly turn them so that they fit in their places.” The next days or weeks you will see the development in the hand movements from rotating the puzzle piece until it fits the cut-out to turning the puzzle piece in the middle of the puzzle board in the correct orientation, i.e. the concept of orientation has developed.

Figure 3.
Figure 3. When playing on the colourful side becomes easy, the black-and-white side is introduced if the child herself does not turn the puzzle board during play.
Children often memorise the locations of the puzzle pieces on the colourful side. If you give a puzzle piece to a two-year-old child, she typically turns the colourful side of the puzzle piece up and then decides where the form should be placed.

Figure 4.
Figure 4. The next step in the development is often difficult, may take weeks, months, even years. To understand that a picture is a representation of a three dimensional object may require a long period of drawing pictures of well-known objects and the puzzle pieces. If the pictures are slightly larger than the puzzle pieces, the task to see the similarity of the form of the puzzle piece and the picture is easy because the edge of the picture is visible next to the edge of the puzzle piece. The key card and the training cards that come with the LEA visual acuity tests can be used in training this phase of matching a concrete form with the picture of the same form.
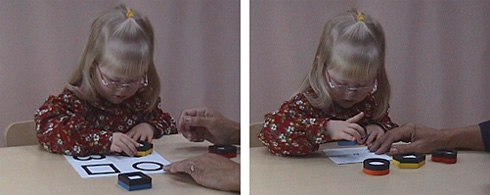
Figure 5.
Figure 5. The next level is to perceive the connection between a concrete form and its picture, first placing the puzzle pieces on large pictures, then on smaller pictures of the Single Presentation Flash Cardstest or pictures drawn by you.
The play can be made challenging by turning the puzzle board 90 or 180 degrees when the child looks elsewhere. When the child is given the next puzzle piece by placing it on the centre of the puzzle board, the child usually starts to place it in the corner where the cut-out has been before, stops in the middle of the movement, looks puzzled for a moment and then jubilant when she realizes that the puzzle board has been turned and the correct cut-out is in a new location. You have collected important information of spatial memory and eye-hand-coordination.
If the large pictures are slightly larger than the puzzle pieces, the task is easier than if the pictures are of the same size as the puzzle pieces. The key card that comes with many visual acuity tests can be used for matching.
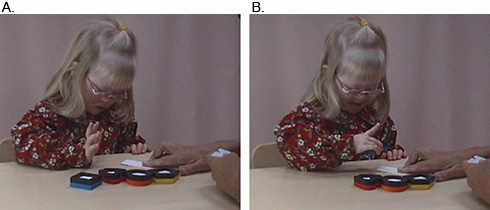
Figure 6.
Figure 6. A. When matching the puzzle pieces with pictures of larger size has become easy, smaller and smaller pictures can be introduced. These smaller pictures can be drawn with the child watching or large pictures of the Playing Cards are used. When the child is accustomed to look at the small pictures of the symbols, Playing Cards are used to measure visual acuity with single symbols. Notice, how demanding the test situation becomes and how proud the child is when she can see the picture.
This test situation is much easier than the tests of visual acuity using line tests because there is no disturbing visual information around the optotypes, the symbols. When near vision acuity is measured with single symbols, the name of the test is recorded in the test results, so that nobody assumes that the child has been tested with a line test.
| A. | B. |
 |
 |
| Figure 7. | |
Figure 7. Measurement of visual acuity of each eye separately requires covering the other eye. There are different patches for this purpose. If the child has spectacles, a thin face tissue folded to a triangle is an efficient cover of an eye. Now the so called “screening frame” is available and is more pleasant than patches; it does not hurt when removed.
If the visual acuity is not symmetric, the use of vision of the weaker eye can be trained by drawing for the child when the child gives the suggestions on how the picture should be drawn. In that situation the child is highly motivated to watch carefully the development of the picture, i.e. is training exact focusing and fixation, which are necessary for good visual acuity. The speed of accommodation seems to be the last function that becomes symmetric with the dominant eye’s function during the training of an amblyopic eye.
| A. | B. | C. |
 |
 |
 |
Figure 8. A - C. When you try to introduce the black-and-white side, the infant may immediately turn the puzzle board to the colourful side demonstrating that he is not yet ready to play with the more difficult side.
When playing on the black-and-white side, a typical two-year-old child turns the colourful side of a puzzle piece up and then decides where the form should be placed.
There is a great variation in the age for development of communication that is necessary during testing. Matching is the earliest response in many test situations. It requires the concept ‘same’, which may be present as sameness of colours toward the end of the first year if a typically developing infant has experienced play situations where objects are sorted in groups based on colours. This creates awareness of categories, a typical function of the visual system. Using this approach, typically developing children can learn to respond in testing of binocular visual acuity as early as at the age of 13 months, although reliable answers are more common first at the age of 18 months.
When playing with young children and children with developmental delays we should carefully choose our sentences to match the vocabulary that the infant/ child is accustomed to. If possible, use the dialect of the family and speak as closely like the parents or the therapist/ teacher of the child as you can. Sometimes it is wise to introduce the puzzle game to the parent or the therapist/teacher of the child and let them start the play. Many children have experienced frightening situations in hospitals where a new person was first nice and then did something painful so they are likely to be on guard not knowing what will happen next.
Since the training and observations may take weeks or months, they should be arranged as a part of the child’s normal play situations. The interpretation of the child’s responses may be difficult to the caretakers. Therefore video recording the child’s behaviours is usually helpful because the responses can be evaluated as many times as necessary by the vision rehabilitation team together with the child's therapist and/or teacher. Although the LEA Puzzle looks like any puzzle, it assesses several brain functions that are used in this task, it is a paediatric neurophysiological test.