Early Detection, Treatment,
and Intervention
of
Problems in Visual Functioning
due to changes in the anterior part
of the visual system,
and/or
in the visual processing functions
Slide 1.
This lecture was given at the World Ophthalmology Conference in Tokyo on the April 2, 2014, in the pediatric session The Child Who Does Not See Well - Diagnosis, Rehabilitation in the Imperial Hotel; speakers included Celia Chen, MBBS, PhD, FRANZCO, Mark Borchert, MD, and Se Joon Woo, MD.
The title stresses the fact that visual problems may occur as a consequence of changes in functions in any part of the visual system. Presently in many countries, infants and children who have changes in the visual brain and, yet, have a normal visual acuity, are not diagnosed as visually impaired. This is because the definition of visual impairment (in the old International Classification of Diseases depicts visual impairment based on visual acuity and visual field only) does not include changes in the visual brain. The number of infants and children with mild or no disorders in the eyes and severely impaired visual functions due to brain damage is increasing rapidly as a result of improved medical care for small, prematurely born infants, severe infections, and trauma that are common causes of impaired vision in infancy.
Visual impairment in children is often present at or soon after birth. If the risk of vision impairment is known, and the infant is observed for symptoms or signs related to problems in visual functioning from disorders in the eyes, in the visual pathways, and/or in the visual brain, visual impairment could be detected and preliminarily diagnosed during the first days or weeks.
During the first year of life, vision develops faster than at any other age. Vision is important in the development of communication, memory, motor functions, and cognitive functions. Therefore, we should carefully observe infants’ visual functions and assess them and start early intervention if we notice a delay in their development.
Slide 2.
Visual impairments of children are often present at or soon after birth. If the risk of vision impairments is known, and the infant is observed for symptoms or signs related to problems in visual functioning from disorders in the eyes, in the visual pathways, and/or in the visual brain, visual impairments could be detected and preliminarily diagnosed during these first days or weeks.
Detection and diagnosis often occurs later than the first days or weeks of life because infants with impaired vision have other more visible problems of functioning due to asphyxia during birth, Down syndrome, other syndromes, deafness, epilepsy, or atypical general development. The vision of all infants at increased risk of vision impairment should have their vision assessed as a part of the first diagnostic work-up. If there is delay in the development of eye contact and early visual interaction, infants with high refractive errors or poor accommodation should receive their near vision glasses within the first few weeks following birth so that their visual communication can start to develop.
In many countries hearing is formally tested at birth; however, assessment of vision is often only an observation of normalcy based on the appearance of the eyes. The first registered observation of the use of vision is in several countries at the age of 6 weeks, latest at the age of 8 weeks, the age at which infants should already have established eye contact with parents, siblings, and caregivers.
Slide 3.
The first visual milestone, initial eye-contact, is not generally considered very important and the parents are asked to “wait and see”. Like the other developmental milestones of the first year it is not considered as a visual milestone but a sign of emotional bonding, which it is as well. Most often, health care providers are concerned with disease detection in initial early assessments.
If we choose the developmental milestones where vision is an integral part of functioning and often forgotten, we have five easily recognizable visual milestones for the first year of life:
- eye-contact
- beginning of enjoyable visual interaction
- visual awareness of and beginning use of hands
- goal-directed-reach and
- face recognition.
Slide 4.
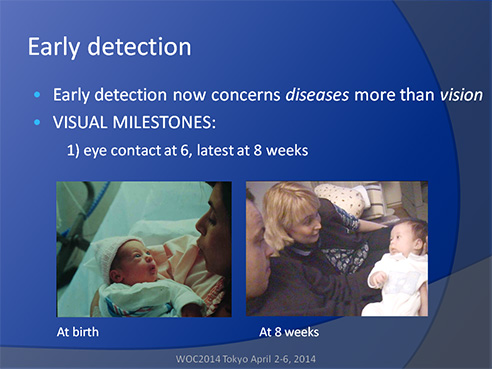
Eye contact between the infant and parents is essential in the development of communication and is experienced as the first bond between them. Eye contact and copying of facial expressions can be present at birth and is expected to be well developed by the age of 6 to 8 weeks. At this time the infant should be able to visually communicate with both parents. In the video the father says, “You try so hard but nothing comes out of your mouth.” In that moment the baby vocalizes and the baby’s voice carries a clear message of something, although we do not understand it as well as we understand visual communication. Then both parents answer, “For sure you can chat.”
If eye contact does not develop, both the infant and the parents experience the lack of contact as a stressful situation instead of the joy of being together. Lack of eye contact disturbs the development of parent-child bonding and can lead to disruption of early emotional development of the infant. Visual communication is a learned function and should start early. The importance of recognition of this delay in the development of vision and need of immediate early intervention was stressed by Patricia Sonksen, a British Developmental Paediatrician in a slide as “Developmental Emergency” in her lectures already in late eighties but published first in 19971. The family needs immediate help in developing communication and bonding. The infant should be kept close to the parents (as in Kangaroo pouch care, KP care) with gentle tactile and auditory communication used to support bonding2.
Communication - at 8 weeks
Visual communication and interaction are the earliest visual functions to observe. If they do not start at 8 weeks, we have VISUAL EMERGENCY.
Slide 5.
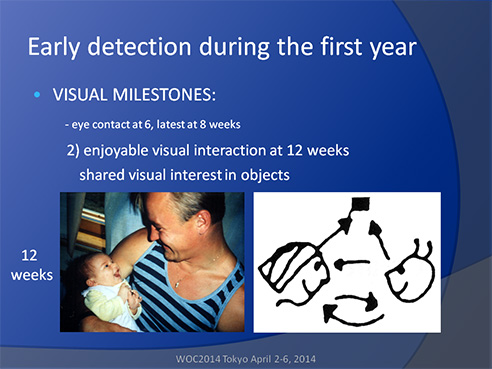
The second easily noticed visual milestone is the lively and enjoyable visual and vocal communication at the age of 12 weeks, often occurring earlier. At this same age, the infant observes the direction of the parent’s gaze and later learns to copy the turn of gaze to an object that the parent looks at while using it. The infant is developing a sharing of visual interest3 and learning to watch the parents’ reactions in numerous situations, which is a beginning of understanding other individual’s emotions and aims. An infant may observe and listen to the mother so intensively that he/she is aware of the depressive moods of the mother before anybody else notices them4.
Mothers and fathers of disabled infants should have their own rehabilitation and support programs in the hospital so that their needs are met already before and especially during the first information on the infant’s diagnosis. In many countries, weekend gatherings and summer camps for children and their families provide peer support. Older children are often more open at the camp fires to talk about their experiences in kindergarten and school, which is very important information to the rehabilitation personnel. Younger children and infants observe the older children and compare their strategies in different tasks and play situations, which is an excellent way to further develop skills for communication and play.
The third visual milestone is awareness of hands and exploring them. At the age of 3 to 4 months infants look at their hands, move, and turn them at varying distances from the eyes. This supports development of stereovision. When the hands happen to meet in the midline, this contact between two parts of the body is important for becoming aware of the body structures. This, in turn, is the beginning of awareness of space. An infant can be helped in this important activity if an adult supports the arms at the elbows and guides the hands to meet at the midline. Usually the infant then brings the hands into the mouth to learn more about the structure of hands.
Slide 6.
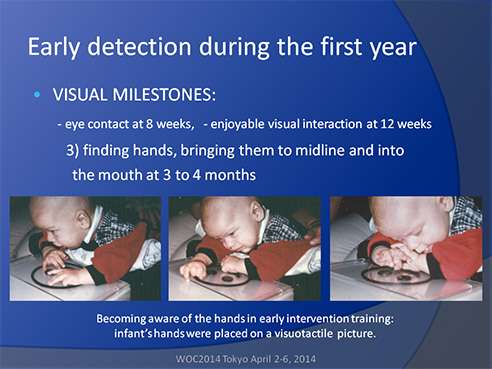
If an infant has not discovered his hands, he/she can be placed on a visuo-tactile object that makes the infant aware of touching something, as seen in the slide above. The middle picture was taken just when the infant noticed his hands: his forehead was in deep wrinkles as if he struggled to focus his eyes to see that “something” that he could both feel and see. Next, the hands were brought into the mouth for confirmation and further exploration of their structure. In these pictures, the visuo-tactile toy was a large picture of a face made by cutting the details of 3 mm thick plastic and gluing them on a clear plastic so that the picture could be used on a light box for infants with limited vision. If you want to create a similar toy, make sure to round the sharp edges of the cut plastic to prevent injury.
Slide 7.
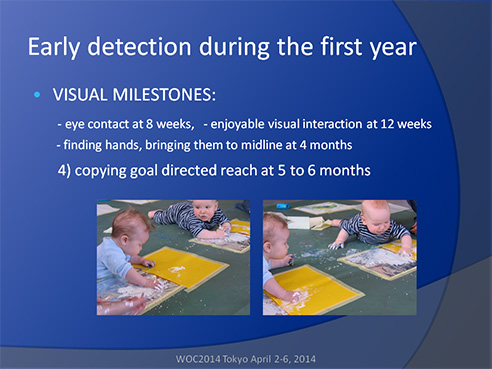
The fourth milestone in the use of vision is the ability to carefully watch goal-directed reach movements and then to copy them by the age of 5 to 6 months. This is possible when the hand movements are reasonably well under control of the infant and the infant has an opportunity to observe other infants and children in their activities. At this age, activities such as painting with yogurt mixed with different colors, is great fun for the infant and the parents observing their infant artist. In these pictures, the infant artists are at the Art Museum of Pori in Finland where this type of early activation of learning began in 20035.
Slide 8.

Infants are fascinated by observing simple eye-hand coordination tasks that are explained when, for example, the adult or an older child is placing a block on another block and then a third on top of the second. If the infant is shown how to push the tower and break it, an interactive play situation is created. Infants also move balls on strings from one side to the other and back, observing their hands (note, these two pictures were not shown at the Conference due to the limited time). Hands are infants’ “second eyes”, i.e. infants receive confirming information through their hands about the concrete structure of objects, their size, surface quality, weight, softness, pliability and what they can do with the objects. If hands have been seen blurred and double, infants do not look at hands and their hands remain inactive and clumsy. By the age of 6 months in typical development, depth perception is well developed and infants learn to understand 3-dimentional forms as a constant, intriguing challenge.
Slide 9.
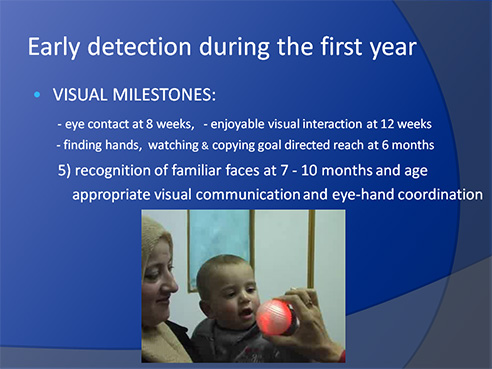
The fifth visual milestone is observable at the age of 7 to 10 months and includes recognition of parents’ and caregivers’ faces and the ability to see the difference between well- and less-known faces of individuals before they say something to the child. Infants have usually developed good visual communication, which we can observe in this short video sequence:
- A short look at the tester as if asking “I can have this ball?”
- An equally short but clear confirmation from the mother that the infant is doing everything correctly.
- A short look at the father outside the picture. Correct copying of the pressing of a small button to change the color of the ball shows good eye-hand coordination.
In less than a minute we have seen age-appropriate, good visual communication and well developing hand functions. This infant has no difficulty knowing who the individuals near him are, even if the parents did not say anything.
If face recognition does not develop , all persons, old and young, need to identify themselves when they approach the child. If the infant sees only a few details of the face or none at all, he/she may turn the ear in front of the mouth of the speaker to hear well and, thus, seem to “avoid eye contact”. This age is one of the most dangerous times in the life of young visually impaired children. If somebody writes in the report that the infant has “autistic behaviors”, the infant may never receive a referral to a pediatric ophthalmologist for assessment and vision will not be included in the early intervention program. The infant may have high refractive error or weak accommodation, which could be compensated by near vision glasses, or the infant may have poor contrast sensitivity and/or motion perception so that facial expressions (low contrast information in motion) are not visible or the infant may have a specific loss of face recognition (face blindness, prosopagnosia). These children are found in all countries at school age without proper glasses because they had a diagnosis of “Asperger syndrome”. In school age we can give spectacles and devices and arrange teaching to fit the needs of the child, but we cannot give back the early formative years. Visual deprivation has caused weak development in learning and in mirror neuron functions that is a specific amblyopia at higher cortical levels than amblyopia due to competition between the images of the two eyes in the visual cortices.
Slide 10.
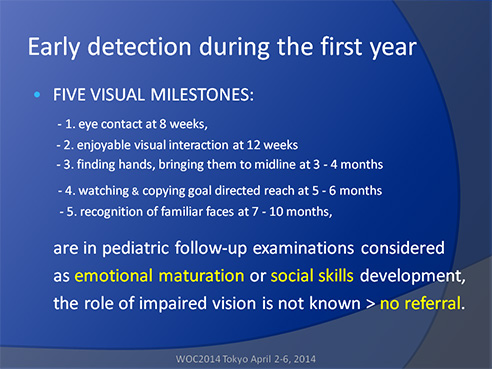
The five visual milestones are not well enough known at the basic health care level and thus observations are thought to be related to emotional maturation and development of social skills without recognizing the role of vision. Because the role of vision is not considered when an infant does not meet a milestone, the infant is not referred to an ophthalmologist and the “wait and see” continues. This is a problem in all countries. Therefore, vision should be included in the teaching programs and in short introductions in questionnaires for each milestone.
Slide 11.
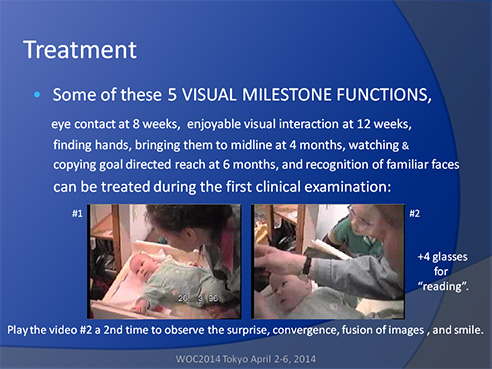
If an infant is referred from the basic health care to an ophthalmologist, sometimes the problem is solved in a few seconds, as in this case when an otherwise normally developing 4-month-old infant refused to look at the face of her mother. Usually bringing hands to the midline brings the gaze to the midline. In this case even this strategy did not work.
The infant was easy to assess because she did not accommodate or converge. Her refractive error was +1 in both eyes. Consequently, the image of the mother’s face at the level of the infant’s retina was blurred and double. When +4 diopter (+3 for the 30 cm distance of the mother’s face and +1 for the refractive error) reading glasses were placed in front of the baby’s eyes, for a moment she was surprised, then she looked at her mother’s face, converged briefly, and then apparently fused the images and smiled at her mother for the first time. In the video you can hear the joy in the mother’s voice when her child looked at her and smiled for the first time6.
Infants who learn to accommodate late may overaccommodate and develop esotropia, often at the age of 6 to 7 months. It is possible to design glasses for most infants, who are detected without delay, to keep the eyes straight at near vision and, when needed to use distance penalization, i.e., blur the image of the squinting eye at distance so that no double images are seen. Infants will usually accept these glasses and thus there is no need for patching or surgery. Later the child can have progressive lenses that are cosmetically better than bifocal lenses. Amblyopia has been prevented from developing.
Slide 12.
Whenever we are worried about an infant’s vision, several clinical tests are available to examine the structure and refraction of the eyes and ocular motor functions. Tests, such as Teller Cards or LEA GRATINGS, are also available to measure sensory functions. With these tests, we can observe infants’ responses to gratings. Because we do not know how the infant perceives the grating lines, the results should not be given as grating acuity values (and in no case as optotype acuity values, which is a common error in clinical evaluation). However, if an infant avoids looking at the gratings, it is a clear sign that the gratings are perceived unpleasant; they may appear distorted to the child.
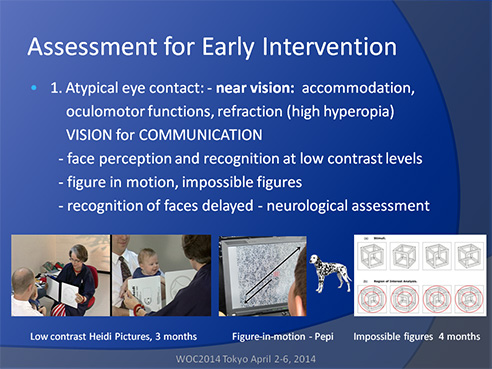
Slide 13.
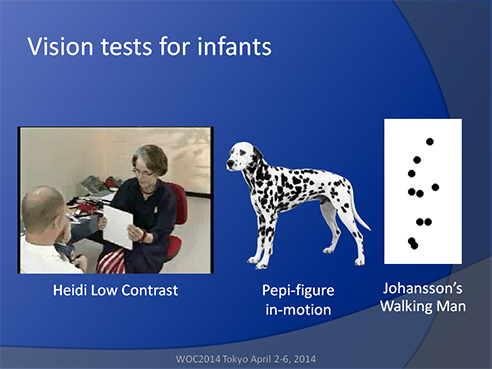
With the low contrast pictures of a smiling face (the Hiding Heidi pictures), we can measure the distance at which an infant recognizes the smiling face and returns a smile, as demonstrated by the 3-month-old child in the video. If the distance at which the infant responds to the smiling face at a 2.5% contrast level is only a few inches, parents and caregivers are advised to use make-up to increase contrast. Even men can use a brown contrast pen – and no mustaches hanging in front of the upper lip. If a visually impaired infant does not see the facial features, is important to help the infant to explore parent’s face with hands and mouth. Normally sighted infants also enjoy touching the face of parent as a part of communication.
The Pepi test at full and lower contrast levels is a figure-in-motion test: the picture of the Dalmatian moves on a background of the spots of Dalmatians and can, therefore, be seen only in motion. Infants at age 4 months enjoy looking at it and, thus we can first observe fixation on the red-white target in the middle of the screen, a quick saccade to the corner when the dog appears, and the tracking movement to the opposite corner. If the infant perceives the dog, it is possible to maintain the infant’s attention to the game for several presentations. Whereas, if the picture is not recognized and the infant perceives only a faint, formless blur moving, the infant seldom tries to follow the movement more than once.
 |
Johansson’s Walking Man interests infants who can perceive the difference between the walking man and a scrambled moving of the spots6,7. |
Slide 14.
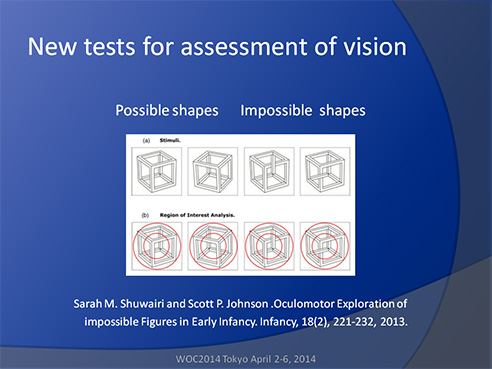
Shuvairi’s “possible” and “impossible shapes” (Necker cubes) also interest infants at the age of 4 months9. When two “possible shapes” are presented to an infant, the infant looks at them in turn about the same length of time the gaze gliding along the lines of the figures. When a “possible” and an “impossible” shape are presented to an infant, the infant spends more time looking at the center of the “impossible” shape (within the smaller red circle) as if trying to figure out how the lines should be understood. At the age of 4 months typically developing infants have depth perception and awareness of 3-dimentional structures. The longer looking time could also be related to novelty.
Slide 15.
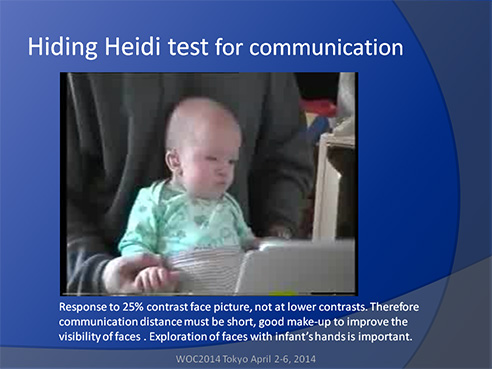
Vision for communication can be difficult to assess if the eyes have unusual structure, e.g. colobomas so that the infant seems to look at the hair line when actually looking at the eyes. With Hiding Heidi test we can measure at which distance the infant can respond to the picture of the smiling face and at which contrast. It is best to start at the distance that the parents have used and felt comfortable. If only high contrast pictures result in a response then adult persons should use strong make up and support communication with tactile communication: the little hands can feel the trembling of vocal cords on the neck and the movements of facial muscles and lips during communication (“baby Tadoma”).
Slide 16.
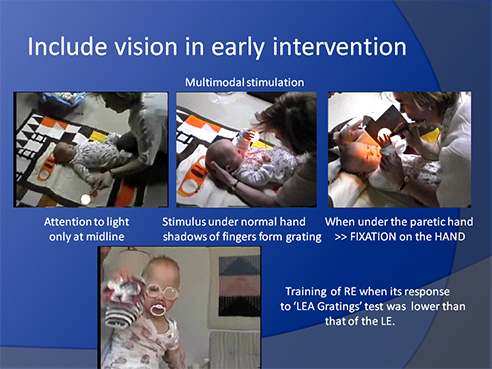
Testing of infants’ vision is important. Even more important is to bring testing to therapy situations where the infant’s neurodevelopmental therapist (physiotherapist or occupational therapist) can function as the tester and, thus, learn how the test situations as play situations can be embedded in the infant’s therapy. This way, use of vision is a part of motor functions in multimodal, effectively activating play situations. An early intervention therapist or teacher for visually impaired children can help the infant’s own physiotherapist during testing so both workers learn about the infant’s situation and can support each other in early intervention. The early intervention therapist/teacher can also explain the strategies that visually impaired infants with several other impairments typically use. An infant who has been in an intensive care unit for several months is accustomed to experience that a new voice is related to a new type of pain during a procedure. Therefore, using as the tester the infant’s own physiotherapist (or occupational therapist), with whom the child is familiar, creates a relaxed atmosphere during the first visit of the early intervention team (in this case a rehabilitation ophthalmologist and a consulting neurodevelopmental therapist of a project on early intervention of infants with multiple problems).
The child’s own therapist was first guided to move the illuminated ball from the side toward the midline of the infant from both sides. This infant shown in the slide responded only at midline. Because the attentional field was so limited, the test situation was continued as a therapy situation (slide in the middle): the illuminated ball was used for activation of awareness of the hands and the attentional field by placing the ball under the better functioning hand of the infant. The ball was a toy ball for kittens and made of plastic with small holes; one of the holes was widened for the penlight. Fingers on the ball formed a grating, which is one of the patterns that effectively activate the visual brain. At the same time, the hand felt the rough surface (tactile information), the form of the ball (haptic information), and the movement of the hand and arm that, in combination, created a multimodal activation of the brain. Next, the illuminated ball was placed under the hand of the less functioning, hemiplegic arm that needed support. Unexpectedly, the infant looked at the hand that was slightly away from the midline. The attended space had increased after a few minutes of activation of visual functions.
A few weeks later when the responses of the right eye to the LEA GRATINGS had started to be slightly lower than those of the left eye, the left eye was patched during neurodevelopmental therapy and a bright, visually activating toy was held in the right hand during training of grasping and moving the hemiplegic arm and hand. Amblyopia did not develop in the right eye.
Slide 17.
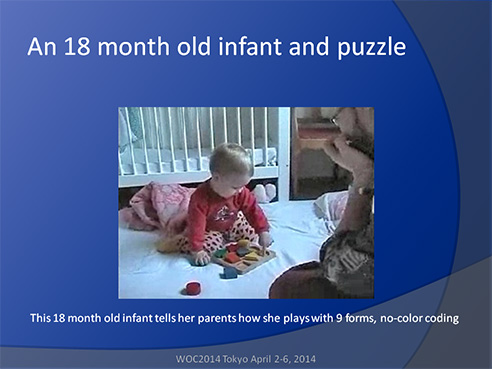
At the age of 1 year, infants become interested in simple puzzles and may even have one-syllable names for the puzzle pieces. At the age of 18 months, infants may play with puzzles that require good form perception. This is the time when an infant can start training for assessment of binocular visual acuity measurement if there are concerns about the development of vision or if the parents want to understand how well their infant can perceive geometric forms, later numbers and letters at an earlier age than those of the routine vision screening.
Slide 18.
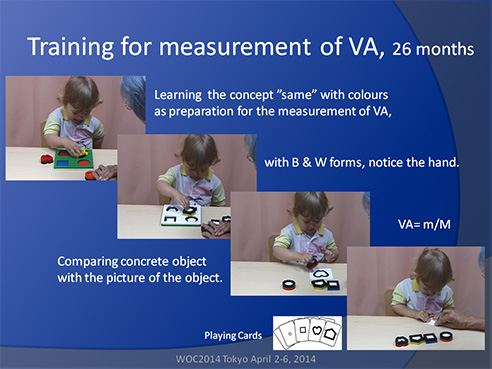
The LEA Puzzle10 is an educational toy, as well as a neuropsychological test situation where we can observe the development of the concept of “same”. We begin with colors and move to black-and-white forms. During the play, we can follow the development of eye-hand coordination and recognition of orientation of objects in space when the infant starts to rotate the wrist for turning the puzzle piece in correct direction before touching it. If we entice the infant to look away from the puzzle, we can turn the puzzle board and observe short-term memory for localization: the child moves the hand to place a puzzle piece in the corner where its cut-out was a moment ago, stops in midair, searches for the correct cut-out, and places the piece in its cut-out – or the child tries to push the puzzle piece with force into the wrong cut-out.
When the use of concrete forms becomes easy, the puzzle pieces can be compared with their pictures. Each picture should be large enough to surround the matching puzzle piece. When this comparison is easy, the pictures can be smaller cards in the LEA Playing Cards test, at which time we are measuring binocular visual acuity in near vision, the most important distance for communication and learning.
The child pictured in the slide had started to use names for the puzzle pieces and spontaneously used the names. If naming is easy, we may use the names. Otherwise, the test situation is best used as purely visual matching.
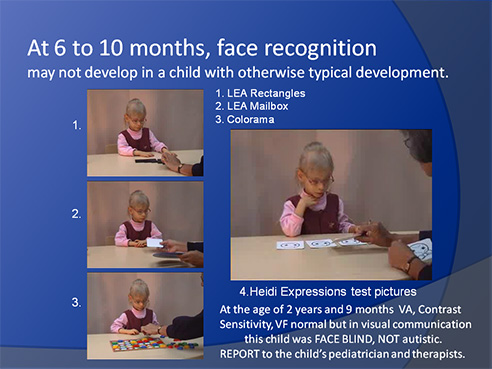
Face recognition, the fifth visual milestone may not develop at the usual age of 7 to 10 months and thorough assessment is mandatory to detect the cause(s) of the delayed development. If the eyes have normal structures and all visual functions, including ocular motor functions and accommodation, are normal, it is possible that difficulties in face recognition are due to a specific loss in the recognition functions. The problem can be a specific loss of visual memory: the infant can see facial structures, can match pictures of faces, but not attach a name to the face.
Slide 19.
Video 1 Video 2 Video 3 Video 4
In the assessment of face recognition it is important to assess early visual processing functions related to basic details in form perception: length of lines and objects (LEA Rectangles Game), directions of lines and objects (LEA Mailbox Game), and situations where the child must use concepts of forms and those of colors simultaneously (Colorama Game)11. Also information about visual closure, Kanizsa illusory contours12, and grating acuity13,14 may add to our understanding of the quality of the visual image that the child uses.
If a child has difficulty perceiving facial structures for comparison of pictures of faces, the child can be assisted by using drawing of pictures of faces together with the child, using magnifying mirrors combined with good make-up of the child’s face to improve visibility, and using tactile information; i.e., helping the child in exploring her face with hands. The child may develop normal matching of pictures of faces, yet recognition of the individuals in the pictures may remain difficult or impossible. A third group of children will not perceive facial structures, which is rare. When asked what they see on the face of the tester, the answer is “skin”, an oval, evenly colored surface. There are usually other losses of functions in the visual brain and elsewhere in the brain of these children, who can be bright and close to typical functioning in many other developmental areas. This makes it often difficult to believe that they are functionally blind in communication situations.
The important feature in the functioning of children with face blindness (prosopagnosia) is that they have to use hearing like blind children to get the emotional color of the communication if they do not see the facial expressions. It takes years of training to learn to be “socially acceptable” and look in the direction of the eyes and pretend having the eye contact that is important to normally sighted people. Sometimes slightly darkened glasses make it easier for other people to remember that the child is visually impaired. The most important thing to remember is that these children are not autistic. They can be aware of other people’s difficulties in understanding them. To be able to handle situations in a mature way requires deep understanding of one’s visual functioning, which should be a central theme through early intervention and rehabilitation at school age so that children learn to function as their own advocates.
Slide 20.

These few slides represent my efforts to depict that the time from birth to age 3 years, especially the first year, are the most important years in the development of vision in normally sighted infants, as well as in infants with atypical development. Thorough assessment of vision is a transdisciplinary effort to follow the development of infants so that all aspects of visual development are understood and used in the care, treatment, early intervention, and education.
References:
- Sonksen P M. Developmental aspects of visual disorders. Current Paediatrics,1997 7.18-22
- Feldman, R.; Rosenthal, Z.; Eidelman, A. I. (2014): Maternal-preterm skin-to-skin contact enhances child physiologic organization and cognitive control across the first 10 years of life. In: Biological Psychiatry 75 (1), S. 56–64
- Nafstad A, Rødbroe I. Co-creating communication. Perspectives on diagnostic education for individuals who are deafblind and individuals whose impairments may have similar effects. Dronninglund: Nord-Press 1999 (Nordic directory for staff in deafblind services).
- Weinberg MK, Olson KL, Beeghly M, Tronick EZ. Making up is hard to do, especially for mothers with high levels of depressive symptoms and their infant sons. J Child Psychol Psychiatry 2006, 47:670–683.
- Hyvärinen L. Vauvan näön kehitys (Development of infants’ vision). In: Setälä P. Vauvojen värikylpy (Color Bath for Babies). Porin lastenkulttuurikeskus – Satakunnan lastenkulttuuriverkosto 2011. Swedish and English editions in print.
- Hyvärinen L. Jacob. WHAT and HOW Does This Child See. VISTEST, Hämeen Kirjapaino 2011, p 11.
- Johansson G. Spatio-temporal differentiation and integration in visual motion perception. An experimental and theoretical analysis of calculus-like functions in visual data processing. Psychol Res 1976, 38:379–393.
- Hyvärinen L, Jacob N. Motion Perception. In: WHAT and HOW Does This Child See. VISTEST, Hämeen Kirjapaino 2011, 99–104.
- Shuvairi, SM, Johnson SP. Oculomotor Exploration of Impossible Figures in Early Infancy. Infancy 18(2), 221–232, 2013.
- LEA 3D Puzzle. http://www.lea-test.fi/index.html?start=en/vistests/instruct/lea3dpuz/lea3dpuz.html
- Colorama Game. https://www.ravensburger.com/us/shop/games/children-s-games/colorama-22057/index.html
- Kanizsa illusory contours. http://en.wikipedia.org/wiki/Illusory_contours
- Hyvärinen, L. Low grating acuity in slow readers with normal recognition acuity. Acta Ophthalmologica 2014. doi: 10.1111/aos.12391
The link to the article is: http://onlinelibrary.wiley.com/doi/10.1111/aos.12391/full
- LEA Grating Acuity Test. http://www.lea-test.fi/index.html?start=en/vistests/instruct/251300/251300.html
The recording of the short talk at the WCO is available at:
http://woc.conference2web.com/content/4150?from_view=all&view_address=
search%3DHyv%25C3%25A4rinen