
Important Information on Measurement of Visual Acuity
Lea Hyvärinen, MD
During my lectures in several countries I have noticed that information on the present standards for measuring visual acuity in population based studies have not been widely distributed. Also the use of visual acuity values in decisions on eligibility for services seems to be poorly known. Therefore this short info.
In September 2003, visual acuity measurement standards for reporting of vision were discussed at the World Health Organisation in Geneva by a group of specialists invited by the WHO and the National Eye Institute (USA). The outcomes of that meeting were published in 2004 as the following document:
The recommendations of this consult group in terms of visual acuity tests are:
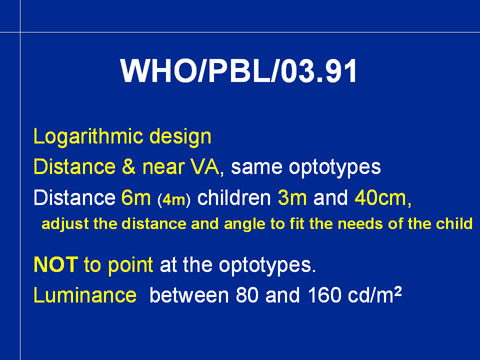
Logarithmic design has been the recommended structure of visual acuity tests used in scientific investigations since middle 1970s. There are, however, a number of older charts with great variation in their structure still in use. The goal is to replace these non-standard charts with logMAR charts in vision screening. This would lead to comparable results in population studies.
Poorly designed visual acuity charts are common in paediatric services and prevent early diagnosis of vision disorders.
Visual acuity needs to be measured at distance and at near using tests with the same optotypes. In a number of countries near vision has been measured with text tests, which does not result in visual acuity values that could be compared with the visual acuity values measured with an optotype test at distance.
Recommended distance for measurements at distance is 6 meters but the 4 meter distance that have been used in many countries for more than 20 years, is unlikely to be changed, mainly because the office rooms are not long enough for a 6 meter chart. For children the test distance is 3 meters. Near vision is assessed at a distance of 40cm (16 inches). When examining visually impaired children, near vision tests should be used at a distance and an angle that give optimal performance.
Optotypes are not to be pointed at but line-by-line isolation and pointing at the line to be read are acceptable techniques to help the person/child to know on what line to read. Pointing at optotypes may facilitate fixation so much that visual acuity with pointing may be twice the value measured without pointing.
Luminance on the surface of the test should be between 80 and 160 candelas per square meter (cd/m2). This luminance level is available in the lightboxes made for measurement of visual acuity. The new technique of using diodes instead of lamps makes the luminance level stable. These lightboxes are durable and can also be used for measurement of visual acuity at low contrast levels.
These recommendations are for population based surveys but the same standard test situations should be used also in clinical assessment and assessment of visual functioning for early intervention and rehabilitation.
Visual acuity and rehabilitation/early intervention
The assessment for services, special education or benefits needs to cover many more measurements. Definition of visual impairment designed for reporting purposes “SHOULD NOT be used for eligibility for services” as stated in the document :
This document stresses “visual impairment in general affects four main functional areas:
ssessment of vision for early intervention, rehabilitation and special education should answer the questions: “How much vision there is for functioning in this activity, orientation, communication etc.” In children it is important also to ask: “Is there enough vision for further development of this function/activity or should the child learn compensatory strategies.”
Measurement of visual acuity for early intervention and special education covers also measurements with more crowded optotypes to detect increased crowding. The functionally important visual acuity value for reading is measured with tests with 25% spacing, i.e. the spaces between the optotypes are ¼ or 25% of the width of the optotypes on each line. As you know, this type of test is available as test #250800 , which has both 50% and 25% spacing between optotypes in the LEA Vision Test System.
In visually impaired children visual acuity measured at different distances and with different tests may greatly vary, as shown in this case:
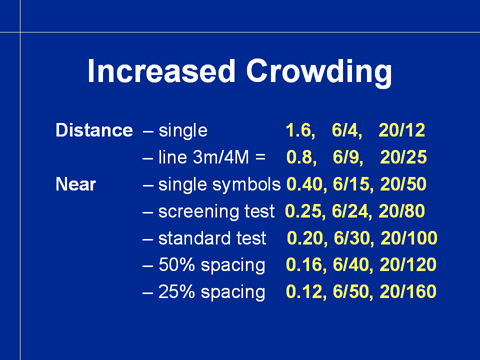
This child, like so many other children came to school with a report stating that his visual acuity was 1.6 (6/4, 20/12) and he was taught as normally sighted until it became apparent that he had great difficulties in seeing normal texts. With the present requirement of measuring visual acuity at distance AND at near this kind of errors will be avoided in the future.
When visual acuity cannot be measured with optotype tests, grating acuity tests are used. The resulting grating acuity values must not be reported as optotype acuity values. When grating acuity is reported as optotype acuity it spreads confusing information in many countries. It should be known that grating acuity values below 6 cycles per degree (cpd) may not be cortical responses but come from superior colliculus. Grating acuity values are regularly better than optotype acuity values when both values can be measured in examination of visually impaired children. The greatest difference that I have measured was grating acuity 6cpd and optotype acuity less than 0.01 (6/600, 20/2000) in a boy who now is adult person and still sees the same way.
This short text covers the questions that I find important to bring to discussion in spring 2005. It is not difficult to measure visual acuity correctly. The LEA tests give you the variation needed for measurement of visual acuity in several different ways so that it is possible to understand how well or poorly visual processing can keep details apart.
LEA SYMBOLS® are the only paediatric test symbols that have been calibrated against the international reference symbol, Landolt C. Paediatric optotypes should not be calibrated against usual letter charts as sometimes has been done because letter charts are not reference charts. Ideal optotypes blur equally, i.e. they are all equally difficult to recognise. This feature is not present in any other set of paediatric optotypes but the LEA SYMBOLS®.
