LEA Flicker Wand
#280000

The LEA Flicker Wand is part of a functional vision assessment to estimate quickly the size of the visual field. For a quick estimate to determine whether major field losses exist, the findings are approximate. For exact measurements, use the flicker and the non-flicker stimulus on an arch perimeter. The luminance of the light can be chosen as 4, 40, or 400 candelas per square metre (cd/m2).
The LEA Flicker Wand is 26.5” (67.3 cm) long. A diode at the end of the flexible wand can be used either as a flickering or non-flickering illuminated stimulus. The 10 Hz flicker results in the largest visual field in infants (Delaney et al 2005).
 |
Handle Button B Button C |
Instructions
During the measurement, the tester observes when the young child’s eyes move from the straight-ahead position to the flickering stimulus of the LEA Flicker Wand.
Older children and adults are usually able to keep looking straight ahead and to tell you when they see the light. If the child/person has communication or motor problems, the rehab/vision team usually finds a technique that allows the child to signal the moment when he notices the light (blinking the eyes, smiling, etc).
- Conduct the assessment at usual room light or low luminance level. Record it.
- Remove your spectacles because the stimulus will reflect from the glasses.
-
Remove the child’s spectacles. If they are strong, make sure that the object to be fixated is well visible without the spectacles or use a sound source.
- Test the binocular, functional field first, then the monocular fields.
-
Tell the child to look straight ahead toward your face if you sit in front of the child. If you stand next to the child, use a fixation target in front of the child, or ask another adult to serve as a fixation target in front of the child, asking the child to keep looking toward her voice.
- Bend the flexible wand in a half circle.
- Stand on the child’s left side so you can see the child’s eyes.
-
Place the LEA Flicker Wand behind the child’s head and bring the flickering stimulus forward on the child’s right side at 40 cm from the child’s head.
-
Bring the flickering stimulus from the back of the child’s head up in the child’s left and right upper field quadrant, and then at the eye level on the left side.
-
Place the flickering light below the child’s head close to the clothing but do not touch the child, and bring the stimulus up in the lower right and left quadrant.
-
To estimate the size of the visual field, notice at which point the child responds to the flicker in all four quadrants.
| A | B |
 |
 |
Figure 1. The tester brings the LEA Flicker Wand forward from behind the child, who is fixating on the face of the tester. A. Stimulus on the right side of the head. B. Stimulus moved above the head. When the child notices the stimulus, the child’s eyes turn to the stimulus with quick saccade.
The LEA Flicker Wand can be used as the stimulus on an arc perimeter, which results in more exact measurements. If measurements at very low luminance levels are needed, the flickering diode can be coved with specific filters to reduce the amount of light. This is especially important in the measurement of the size of scotomas in retinitis pigmentosa to test whether the size is larger at a specific low luminance level. Flickering stimulus is often perceived within scotomas that have been measured with a non-flickering stimulus of the same mean luminance. Combining different measurements of the visual fields, automated, Goldmann, and micro perimetry, it will be possible to detect small variations in the structure of visual fields.
Visual field measurements for early intervention and rehabilitation
One of the corner stones of early intervention and rehabilitation is that the patient’s family and, when the child is old enough, the child him- or herself knows what the condition is and learns to live with it. Without this knowledge the children and youngsters and their families cannot participate in planning their future. Also paediatricians, neurologists, teachers and therapists must get accurate information that they can understand to use it in everyday situations.
We have a new demanding situation in the measurement of visual fields: the possibility of gene therapy in some inherited retinal diseases. All clinical measurements should be made far more carefully than presently. Among the clinical tests, the results of usual visual field measurements of children are “the least reliable”. In many hospitals and private offices of eye doctors visual fields are not measured before the child is 9 to 11 years old. The treatment should be started quite early; therefore the measurements could and should be started well before school age so that the variation of visual functioning is documented in detail. This requires several measurements before the treatment is started.
The present difficulties in perimetric tests are quite apparently related to inadequate communication and use of automated perimetry that cannot be adjusted to the ocular motor and attention functions of many visually impaired children equally well as the manual perimetry using Goldmann and other similar perimeters.
Use of the perimeter tests requires explanation of the test situation to child and the child’s interpreter when an interpreter is used. If both the interpreter and the patient are new, it is advisable to demonstrate the test by first briefly measuring the visual field of the interpreter. This gives the patient an opportunity to observe what happens during the measurement and it makes it much easier for the interpreter to describe the testing situation to the child.
If the parents of the child’s classroom teacher are present when visual fields are measured they can themselves see at which distance from the midline the child responded to the visual stimulus.
The state of adaptation of the retina is the most difficult variable to standardize. If the child has been in bright sunlight the day before, the effects can often be noticed in the retinal functions of patients still the next day. Therefore the luminance levels where the children stay during the day before and during the morning of the day of examinations should be clearly stated and followed to the letter. The visual fields should be measured as the first tests using several test techniques and starting with tests at the lowest luminance levels.
For details in the measurement of visual field scotomas, please read the Chapter 5 in the WHAT and HOW Does This Child See?
References:
Hyvärinen L, Jacob N. WHAT and HOW Does This Child See? VISTEST, Hämeen kirjapaino, Tampere 2011.
Hyvärinen L, Lindsay Gimble, Sorri M. Assessment of Vision and Hearing of Deaf-Blind Persons. Royal Victorian Institute for the Blind, Burwood Educational Series, Burwood, Australia, 1990.
Also: www.lea-test.fi, Deafblindness.
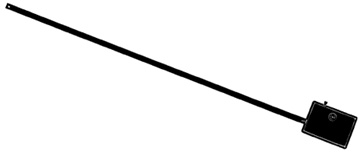
Figure 2. Blinking stimulus that can be turned on and off was a good test target for confrontation field and as an introduction of visual field testing. This device was produced at the University of California, Berkeley, School of Optometry in 1987 for the project on communication during clinical examination of deaf-blind patients, Assessment of Vision and Hearing of Deaf-Blind Persons. The present Flicker Wand is a technically advanced version of this simple test.
Delaney SM, Dobson V, Mohan KM. Measured visual field extent varies with peripheral stimulus flicker rate in very young children. Optom Vis Sci 2005; 82(9):800-806.[ Instructions I Paediatric Vision Tests I Vision Tests ]
This document was last modified on