The areas to be assessed
The assessment has to be organised to meet the individual needs of each child. Some features are common to all assessments:
1. The general state of the child: every child needs to be observed at different levels of wakefulness. The first observations should be made when the child is at a high level of wakefulness and feeling well and relaxed. The child's spontaneous activities are observed before approaching the child. Any motor problems are noted and their effect on the assessment given attention to. Hypotonic children often have better control of their oculomotor functions when standing supported in a well fitted stand. If head control still requires too much concentration, different ways of supporting the head should be tried to find one that is acceptable to the child. Such an "unrelated thing" as the type of supportive shoes used during assessment of vision may influence oculomotor functions - via their influence on whole body tone. The child's occupational or physiotherapist should help in finding an optimal position in the beginning of the first assessment and also later but visual functions need to also be evaluated in the positions in which the child spends much of his/her time during the day.
2. Oculomotor functions, eye-hand co-ordination and the child's level and techniques of communication are assessed first in the same way as they are assessed in low vision children without other impairments (PART I). If grasping is difficult, eye-hand co-ordination may be observed when using toys on a lightbox. In this pleasant play situation the child's eye movements may be better controlled than later when the visual task becomes more demanding during measurement of visual acuity, reading acuity etc.
3. Refraction is equally important as in children without other impairments. In multi-impaired children the measurement of refractive error and prescription of glasses is more often not taken care of than in other children. Try to get information from the child's doctor on both the basic refractive error and the type of corrective lenses used. Since so many children have problems in the development of accommodation, information on measurements of accommodative power should be requested from the child's doctor. If the measurements have been unsuccessful or have not been made, observations on the child's behaviour when using near correction and without it are necessary.
In children who can communicate in the measurement of visual acuity, differences in the values measured at distance and at near may reveal problems in accommodation.
In children who have extension spasms, the spasm may involve the ciliary muscle. Often there is overconvergence, eyes turn to the inner corners of the eyes, and simultaneous accommodation causing transient myopia of 10-15 diopters that blurs everything beyond arm's length.
4. In the measurement of visual acuity, special attention is given to the crowding effect. Visual acuity is measured with single symbols, line test and crowded near test to find out, whether there is difference between these three measurements. It is common that a child with posterior pathway damage has
| single symbol acuity | 0.63 (6/9.5, 20/32), or even 1.0(6/6,20/20) |
| line test acuity | 0.32 (6/18, 20/60) and |
| with crowded symbols | 0.12 (6/48, 20/160) or 0.06 (6/100,20/330). |
5. Even if optotype acuity can be measured, grating acuity may be interesting to know when optotype acuity is low because grating acuity depicts resolution of lines in a large area. It can be measured using grating acuity cards or the LEA GRATINGS. In developing countries grating acuity cards are problematic because they do not tolerate humidity or dust and are rather heavy to carry. With the simpler LEA GRATINGS similar information can be gathered as with the grating acuity cards. For details on the measurement see the test instructions.
6. Contrast sensitivity measured with the optotype tests may have decreased more than visual acuity. Contrast sensitivity measured with grating tests may be much better than that measured with the optotype tests. Both measurements are therefore of value.
The communication sphere of the child can be quickly assessed using Hiding Heidi or your own face. In testing of school age and older pre-school age children, the child can point to the picture. Sometimes the test has to be made to a game to entice the child to respond: one person holds the blank card and the other person the Heidi picture and the child tries to find out who has the Heidi picture. Often waving bye-bye to Heidi is more fun than simple pointing.
When contrast sensitivity is found to be low, the finding needs to be explained to the child's teacher but also to persons who can see that the child will get light coloured food on dark plates and dark coloured food on light coloured plates and that poor quality copies of text are not used etc.
7. Colour vision may be lost in a number of cortical lesions either due to localised lesion in the area of colour analysis, due to diffuse lesion in the primary visual cortex as in carbon monoxide poisoning or due to lesions of the optic nerve. However, in most cases there is intact colour vision for primary colours at least.
8. Visual field defects are either half field defects, quadrant defects, central scotomas due to damage to the macular projection area in the primary visual cortex or 'Swiss cheese' like field defects because of patchy loss of fibers in the optic radiation. The extent of the visual field can be found out with confrontation visual field, and more exactly with Goldman perimetry. Central scotomas can be plotted with either Macular Mapping test, Damato campimetry or may be measured at the eye clinic using automated perimetry.
It should be clearly understood that dark spots visible in the visual field recordings do not truly depict the visual field of the child. There are rarely any dark spots in the child's subjective visual field. When no information arrives to a certain area of the visual cortex, the connections between the cortical cells are rearranged and the previously quiet area is taken over by information from the adjacent areas. Therefore the blind spots disappear and subjectively there is only some distortion of straight lines if a grid is carefully studied with the child. The small scotomas should also be carefully looked for in the reading field because they may lead to disappearance of only 1-2 letters and thus cause misinterpretation of words or they may now and then happen to be located at the point of the next fixation and thus the fast eye movement to the next reading location is misguided.
9. Visual information related to motion is transferred through the magnocellular route which uses only a limited number (10%) of the optic nerve fibers. Changes in motion detection and discrimination are not measured during clinical examinations because there are no routine paediatric tests available. The test methods are developing and will increase our understanding of visual functioning when they are used clinically. Simple observations may reveal the child's problem. Ask the child to look at you when you first sit still and then move your head from side to side and up and down. The child may be able to tell you that your face becomes blurred or even disappears. An older child can be asked to count fingers when they are moved in front of him/her slowing the movements until the child can count them. When the child is moving in a room he may use tactile techniques to verify the location and stop to look. When moving in a crowd the child is likely to cling to an adult. Such a child needs long cane techniques despite otherwise useful vision.
Motion detection and discrimination can be lost because of retinal lesions, pathway lesions, and/or at the cortical level, either at the primary visual cortex or in parietal functions. In the functioning of the child this can present itself either so that the child sees only objects in motion or only when they stop moving. This can be observed during ball games and when testing tracking movements. If the child does not follow the moving target but makes an accurate saccade to it when it stops, the child either does not have tracking movements or does not see the movement. The child may be able to explain that the object disappeared and then reappeared (= visual problem) or that it was difficult to keep looking at it when it moved (= motor problem). Sometimes the child may be able to follow the movement when moving the object him/herself. Another problem in motion perception is loss of perception to objects that stand still but become visible when they move. This can lead to that a child constantly moves the text that (s)he is reading, even if it is magnified with a CCTV to 'optimal size'. Movement of the text causes nausea in adult teacher's aids and parents who may try to stop this 'strange behaviour'.
10. Lack of stereopsis is not a major loss of vision. Stereopsis does not develop in quite a number of normally sighted individuals who are totally unaware that their vision is in some way disordered. In visually impaired children lack of stereopsis is nearly the rule, because development of stereopsis requires quite good vision in both eyes and good binocular functions during the first year. In children, who developed normal vision before they lost their stereoscopic function, loss of stereopsis causes problems in eye-hand co-ordination during several weeks or months until new techniques in reaching are learned.
11. Changes in cognitive vision or agnosias may involve any type of recognition. The most common difficulty is loss of recognition of faces, either in real life situations or recognition of faces in pictures.
Difficulty in recognising faces may be related to several functions:
- a child cannot see the low contrast details of facial features (= problem caused by the quality of the image, i.e. anterior pathway problem),
- a child can see the features but cannot keep them in memory long enough to recognise them, or
- a child can see the features and keep them in short term memory for a limited time but not get them into long term memory.
- a child cannot see faces when people are moving and this is misinterpreted.
Sometimes the child can keep visual information related to faces only in the immediate memory. Then it may happen as once happened in my office: A girl did not seem to have any difficulty in knowing the difference between me and the therapist, although both of us had white clothing and dark hair. I had to go to another room for less than two minutes. When I came back the girl asked me "Are you the same doctor who was here before?" as if she had only immediate memory of faces. She has not learned to recognise her friends by facial features but by voice, yet she recognises her parents in a group of adult persons.
 Some children recognise familiar faces but have difficulties in interpreting facial expressions. This can be evaluated with the Heidi Expressions Game and when playing different characters. The expressions on the tester's face and in the Heidi pictures are compared and the child is encouraged to try to make the same expressions. If the expressions are not learned through visual copying then tactile information is used to teach the basic expressions. After that the Heidi Expressions pictures can be used again. Of each expression there are three cards, two that are identical and a third where Heidi has a bow. If the child does not recognise the expressions (s)he often matches the pictures where Heidi has a bow.
Some children recognise familiar faces but have difficulties in interpreting facial expressions. This can be evaluated with the Heidi Expressions Game and when playing different characters. The expressions on the tester's face and in the Heidi pictures are compared and the child is encouraged to try to make the same expressions. If the expressions are not learned through visual copying then tactile information is used to teach the basic expressions. After that the Heidi Expressions pictures can be used again. Of each expression there are three cards, two that are identical and a third where Heidi has a bow. If the child does not recognise the expressions (s)he often matches the pictures where Heidi has a bow.
Visually impaired children may also have loss of low contrast information as the cause of not seeing facial expressions. The six basic expressions are therefore printed at 10% and 2.5% contrast to evaluate the role of contrast.
In the case of total loss of facial recognition, children usually learn to use other features, e.g. clothing, to recognise people. Then incidents like the following are possible: Because of a cool summer evening, the mother of a child with loss of facial recognition had her husband's flannel shirt on top of her blouse. The son came to her and called her "father", which of course was upsetting to the mother and the child.
Inability to recognise objects in pictures may be total or restricted to pictures where an object is depicted from an unusual angle or partially covered by another object. If a child has lost cognitive visual functions to recognise objects in late pre-school or in school-age, he may also be unable to copy the pictures even if the picture is next to the paper so that there is no memory function involved. However, when asked to draw an object that the child knows well, like a ball or an apple, the child may be able to retrieve the image from long-term memory and draw the picture. Thus the concept is there but the ability to visually recognise is missing.
12. Difficulties in recognition of size or length, based on visual information can be detected in a play situation. When the Rectangles Game is used, a two-year-old can usually point to the right rectangle when one asks which one is longer.
 If the child does not understand the question, the concept of bigger/smaller is trained by using haptic information, by allowing the child to measure the sizes with his/her hands. If the child develops understanding of size differences based on haptic information but does not seem to understand the differences in sizes through visual information, there is specific vision impairment of recognition of sizes.
If the child is unable to see the length of the rectangles he/she is asked to grasp the rectangles one by one in the longest direction stacking them according to size or colour. If the grasp is adjusted to the correct length of the object well before the fingers touch the object, then there is visual information for planning the grasp (dorsal stream information) although the child is unable to analyse the form visually (ventral stream function). Organization of movement with respect to the visual world is a function of the dorsal pathways.
If the child does not understand the question, the concept of bigger/smaller is trained by using haptic information, by allowing the child to measure the sizes with his/her hands. If the child develops understanding of size differences based on haptic information but does not seem to understand the differences in sizes through visual information, there is specific vision impairment of recognition of sizes.
If the child is unable to see the length of the rectangles he/she is asked to grasp the rectangles one by one in the longest direction stacking them according to size or colour. If the grasp is adjusted to the correct length of the object well before the fingers touch the object, then there is visual information for planning the grasp (dorsal stream information) although the child is unable to analyse the form visually (ventral stream function). Organization of movement with respect to the visual world is a function of the dorsal pathways.
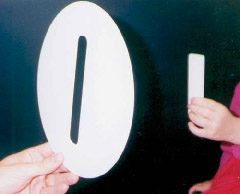
13. Recognition of direction can be tested in the following play situation: Use the Mailbox Game with the slit in the middle. First the slit is shown to the child in different orientations and the child is allowed to study the slit in different orientations by moving his/her hand in the slit.
If the child understands the concept of different orientations the child is asked to drop a card or a small envelope through the slit while the slit is presented in different orientations. Watch beginning of the movement: the card starts to rotate to the correct orientation before half of the distance to the mailbox is used. If this happens there is vision to guide hand movements. We should be aware that in some visually impaired children wrist movements are not well developed partially due to lack of training related to insufficient visual information for incidental learning. There may be also primary motor problems involved.
14. Changes in the function of the parietal lobe may cause loss of egocentric orientation. Vision cannot be effectively used for guidance of movements, the child's motor functions look clumsy although basic motor functions as such are normal. This may lead to a condition that is a mirror image of that described in the previous paragraph: the child may be able to visually define whether lines are horizontal, vertical or tilted but cannot turn the envelope to the orientation of the slit when trying to drop it. It requires an experienced physiotherapist or occupational therapist to assess that the motor functions are there but that they are aimed incorrectly in visual space as if limited or poor planning is taking place. If there is also impairments of motor function the role of loss of parietal lobe vision is very difficult to assess. Some such children seem to be poorly aware of their body when using either visual or tactile information.
Eye hand coordination may also be disturbed because of irregular visual feedback loop during movements: the child looks at an object, turns his/her head away and then reaches for the object. In this situation we may suggest the child to close eyes instead of turning the head and compare the quality of movement when the eyes are closed to when the child is asked to look at the hand reaching for the object. If the movement is smoother with eyes closed, then that is the better technique to be used - despite the fact that it does not look 'normal'.
15. Recognition of places can be affected two different ways:
The child may find it difficult to remember details that can be used for recognition. In this case it is important to assess whether these details are seen clearly enough at the distance where they are critical (=does the basic vision impairment prevent recognition). Enhancing the image by magnification or by adding high contrast details for identification may help the child to overcome such difficulties.
The child can see details of the environment but cannot understand the spatial connections. Such a child may walk on "paths" along the walls and furniture using both visual and tactile landmarks like a severely visually impaired child who has anterior vision impairment. The child may also be unable to diagonally cross an open square space, the sides of which he/she has studied by moving around.
Some children can get lost in their own living room if any pieces of furniture have been moved. Other children may have a phobia of moving from one space into another. Tasks like walking through a gate or through a ribbon curtain in a door way may be impossible.
16. Level differences between two surfaces are normally perceived quite early. Some children do not learn to assess depth in this way and are frightened by a level differences of a few centimeters. They are also unable to tell whether a change in floor surface is accompanied by a step or not. They stop at shadows and thresholds and touch with their foot to find out whether there are level differences.
17. In the case of problems in simultaneous perception, simultanagnosia, attention cannot be directed to different parts of a picture or a group of objects but can cover only one thing at the time or sometimes only small details of an object. It makes formal testing of visual fields impossible in some cases. Measurement of visual field is often the least popular test situation among children with CVD. In an observation situation it is advisable to use sound as the target in front of the child, e.g. a person talking to the child behind a screen while bringing the objects from behind the child. This requires that the child can simultaneously attend to visual and auditory information. These children require observation of the use of peripheral vision in orientation and mobility and observation of strategies used for near vision tasks for the assessment of the function of the central visual field. Looking through railings at a distant target, e.g. at the zoo, can prove difficult for some children who only appear to be able to see the railings but nothing beyond.
18. The oculomotor and other motor abilities of the child were assessed in the beginning of the assessment. Any problems in motor functions that occur during testing should be discussed with the child's ophthalmologist and neurologist. Because they are complex and require demanding test situations they need to be analysed further by combining the results of clinical examinations and video documentation of eye movements, eye-hand co-ordination, and fine and gross motor skills in play and therapy situations as a part of functional assessment. It is crucial that all motor functions are thoroughly investigated.
If the child's head control is poor, the use of glasses becomes ineffective when the head hangs down and the child looks over the glasses. The child does not see at the level reported by the doctor but as if (s)he had no glasses.
When reading from the black board or when sustained near vision tasks require the child's total concentration and strength, control of posture may be lost and the child can sink into a tilted posture that effectively prevents optimal use of the limbs. Many myopic children and children with vision impairment caused by lesions in the anterior visual pathways commonly use a short reading distance, which increases flexion spasm and may disturb the use of hands. As such ergonomic problems are so common among these children they need to be observed for extended periods both in the classroom and at home, to find the ergonomically best optical and non-optical devices.
During therapy and teaching, observation of eye movements may reveal periodic disturbances that are later proven to be related to abnormal brain activity, caused by a form of epilepsy without obvious fits. In other cases loss of control of eye movements may be related to simultaneous disturbance in gross motor functions. Video recording of how the child functions in therapy and classroom situations usually prove very informative helping the team to understand the child's strengths and weaknesses.
Difficulties in fixing the eyes on a chosen target need to be carefully observed. The period of fixation in some children can be very brief affording insufficient time to perceive longer words. Some children cannot fixate at all, the gaze wanders from one object or picture to the next without the child being able to make stops for fixation. Observation of the eye movements through a transparency when the child is looking at pictures or is reading provide the most practiced method, because the alternative methods recording of eye movements or using the expensive scanning laser ophthalmoscopic evaluations are only available in a few academic establishments.
19. Visual memory may be affected in many different ways. It may be so short that the child cannot remember a picture or an object for more than a fraction of a second. The child may recognise the picture by naming or matching if two or three pictures are next to each other but may not be able to, if they are presented after each other. Such a child may also be unable to copy pictures from the blackboard because he forgets the picture while shifting the gaze from the picture to the paper.
The above mentioned visual functions should be assessed before the neuropsychologist starts his/her tests so that enough information is available for selection of tests that measure visual closure, object-background concept, scanning techniques etc.
 The child may be able to properly turn the wrist to put the envelope into the slit although he/she was unable to define the orientation of the slit visually. This part of the test often requires another adult person who pretends not to understand what to do when asked to turn the card in the same orientation as the slot and asks the child the orientation is correct 'this way or that way'. The child may not be able to 'understand' this part of the test after several training sessions (ventral stream function) although (s)he uses the concept of orientation of lines based on information of the position of the hand.
The child may be able to properly turn the wrist to put the envelope into the slit although he/she was unable to define the orientation of the slit visually. This part of the test often requires another adult person who pretends not to understand what to do when asked to turn the card in the same orientation as the slot and asks the child the orientation is correct 'this way or that way'. The child may not be able to 'understand' this part of the test after several training sessions (ventral stream function) although (s)he uses the concept of orientation of lines based on information of the position of the hand.
Previous Chapter 
|
 Next Chapter Next Chapter
|