HOW TO DETECT IMPAIRED VISION IN INFANTS AND CHILDREN?
Impaired vision may affect a child’s general development and the whole family if the early intervention does not start really early. Therefore detection of vision impairment is important and availability of early treatment and (re)habilitation (early intervention) should be high on the list in the development of paediatric medical services. For planning detection of deviations from normal vision development we need to know how vision may deviate from normal. The most common deviations are discussed in this information for paediatricians and public health nurses.
In vision screening we have two goals:
- to find children who are visually impaired, a small group (<1%) among healthy looking children and 20 to 80% among children who have other more noticeable impairments.
- children with strabismus and/or amblyopia or at risk of developing them (2-4%).
Since more than half of visually impaired infants have several impairments that affect their activities, we have a third area of vision screening:
-
visual impairment should be specifically sought in children with other impairments: motor impairments, developmental delay and hearing impairment, by referring all infants with impairments to ophthalmologic examination with a special question on vision and refraction, not only structure of the eyes. Small prematurely born infants are a new group that should be carefully followed to detect vision losses typical to them.
Healthy children with amblyopia or strabismus can be treated in many countries, although not in all. Several types of strabismus and amblyopia can be prevented or corrected by using spectacles and thus surgical interventions are avoided. In countries where infants and children may get spectacles, early detection of deviations from norm is therefore mandatory. Detection of deviations is most effective as a part of visits to health care stations or doctors’ offices for vaccination during the first year. Later vision screening of all healthy children at the age of 4 years and at school is an effective way of securing optimal visual functioning in children.
In most countries vision screening is in the hands of health care workers: public health nurses and their aids; in other countries general practitioners and paediatricians should screen for sensory impairments as a part of their work.
Parents of young children should get information on child development and its deviations from norm to be motivated to bring their children to the nurse or the doctor when they notice something unusual in the child’s eyes or visual functioning.
This lecture was given in 2001 in and updated in September 2010 to add the changes that had happened in the last ten years.

The International Classification of Functioning, Disability and Health, Children and Youth Version (ICF –CY 2007) is the foundation of our work in early intervention and rehabilitation. It requires assessment of functioning in nine activity areas, domains, which are the same as in the ICF for adult populations. Five of them form the Core Domains that are the same as in the earlier WHO publication 93.27 Management of children with low vision. It was created during the meeting of representatives of WHO, several invited advisors to WHO and representatives of ICEVH (now ICEVI) before the world conference of ICEVH in Bangkok 1992. Its name refers to the need to improve services for children with low vision; blindness was never questionable and the services for blind children were well known and usually fairly well provided.
The important content of the WHO 93.27 publication and the ICF-CY is that they recognise the difference between classification of vision impairment for population-based surveys and assessment of visual functioning for rehabilitation services and special education. They require assessment of other visual functions than only visual acuity and visual field and stress the important fact that vision disability is task/activity depended.
A child with impaired vision often functions like a severely impaired individual in some tasks, like a mildly impaired in other tasks and like a child with normal sight in some tasks. This confuses people who do not know the nature of impaired vision causing them to say that the child “sees when he wants to”, which is seldom true.

The ICF for classification of functioning in adult people lists several functional areas that need to be considered: learning and applying knowledge, general tasks and demands, communication, mobility, self care, domestic life, interpersonal interactions and relationships, major life areas, community, social and civic life.
Only five of the functional areas, domains of the ICF, are functional areas of infants and young children. These five are the same as where used in the WHO 93.27. It recommends assessment of vision in four main areas of functioning of children that exist in all cultures and in all age groups:
- Communication
- Orientation and movement
- Activities of daily living (ADL)
- Sustained near vision tasks like reading and writing.
Communication included also interaction, the fifth of the five Core Functions of the ICF.
Visual functioning and abilities need to be assessed in each of these four areas so that we have a good foundation for planning early intervention and special education services.

To emphasize the importance of assessment in each of the four functional areas we have in Finland used this picture of the four-leafed clover since early 1980s (Hyvärinen 1985). In countries where clover grows, finding a four-leafed one among the usual three-leafed plants is thought to be a good omen or to bring good luck. If we remember to consider all four areas of visual functioning, it means really good luck for the child.

This graphic presentation of variation in visual functioning of children (and adult people) with vision loss is the most exact way of describing the nature of impaired vision. As we see here, this child with central scotoma is severely visually impaired in reading and other sustained near vision tasks that demand good recognition acuity but in other tasks (orientation and mobility, O&M, and activities of daily living, ADL) has enough vision to function like a fully sighted person. These situations where visual functioning is fair or good, the tasks are often related to use of the more peripheral parts of visual field where the function is quite normal. Even in normally sighted, the form perception is less accurate in the peripheral vision than in the central visual field. Other children may have normal central vision but limited visual field and among the children who have brain damage all usual clinical measurements may show normal values and yet the child is severely visually disabled.

In the detection and assessment of impaired vision we need to be aware of the fact that more than 60% of children with vision problems have at least one other impairment or chronic illness that affects their functioning. Therefore the groups of children where detection of impaired vision is most likely are the children with other diagnosed impairments. The largest groups are:
- children with intellectual disabilities
- motor impairments, especially cerebral palsy (CP) and
- children with hearing impairment, both peripheral and central hearing impairments and
- children with some syndromes (or) and some chronic illnesses.

In most developed countries there are recommendations for practices to detect deviations from normal development of vision. The goal of early vision screening is to detect the few children who need to be operated early for cataract, glaucoma, abnormal eye lids or, most rarely, for tumours and to detect infants and young children who need spectacles already as young infants or are at risk of becoming amblyopic.
With the increasing number of infants with brain damage related vision loss it is important to be aware of the symptoms of unusual visual interaction and lack of reaching the usual milestones in visual functioning. The observations to be made should be embedded in the basic health care services. The nurses and doctors in charge of them shoud have the tools and the knowledge for observation of each milestone.
The workers in the day care, therapists, teachers and the families should also be aware of such facts as constant strabismus being an abnormal condition at all ages, that infections and inflammations need to be treated also in young infants and that delay in development needs to be investigated. The “wait-and-see” attitude is not acceptable.
The early development of vision and its deviations from norm are followed in many countries using modifications of the list in the pdf you may keep on the wall for quick checking when you examine young children.

Shadows in the red reflex may be caused by cloudiness of the cornea, opacities in the lens (as in the picture to the left), dislocation of the lens (picture to the right) or vitreous floaters or remaining foetal structures in the vitreous. Infants with a large shadow in the red reflex need to be referred without delay to an ophthalmologist who can operate infantile cataracts, if that is the local policy. Monocular cataracts are not operated everywhere because the very demanding postoperative care, patching of the healthy eye and training of the operated eye, cannot be arranged. If the shadow is small and dilatation of the pupil can be used, operation may be postponed if the condition of the baby is not good enough for operation. There is thus variation in the care dependent on availability of surgical care, possibility of arranging the postoperative care and the general health of the infants.


Eye contact is an emotionally important function that may be present during the first days of life. Some new-born infants may copy even the basic expressions.
At the age of 8-12 weeks social smile and effective interaction between infants and their parents is expected.

Video

Deviations from normal development can be noticed during visits to health centre for vaccinations as in this case. The infant had no eye contact, seemed to actively avoid eye contact. This behaviour was present also when the infant was examined in the ophthalmologist’s office. Dr. Lea diagnosed lack of accommodation and tested the child’s functioning when the lack of accommodation was compensated with ‘reading glasses’, i.e. glasses that gave clear image on the retina of the infant. Immediately, the infant had eye contact with her mother and a normal social smile (video).
Whenever early communication/interaction is not normal, sensory functions need to be thoroughly assessed, in vision also accommodation.

Large, “beautiful” eyes that are growing faster than usually should be detected in the basic health care services. Increased pressure may cause photophobia and tearing, sometimes rubbing of the eyes, which sometimes have been diagnosed as symptoms of allergic conjunctivitis. The diagnostic feature is the abnormally increasing size of the diameter of the iris.

Retinoblastoma is a life-threatening tumour that may be present at birth but more commonly starts to grow in infancy or before school age. It is often detected first when it is visible as a white mass in the pupil or because the infant/child develops squint in an eye that has been well aligned for several months.
Sometimes an abnormal red reflex in a photograph brings the family to the eye doctor, as in this picture where the light is reflected from the optic disc, not from a tumour. Similarly the red reflex may be nearly white, if an eye has inward squint of 15-20 degrees (light is reflected from the disc) or there is coloboma, loss of a part of the retina, so that the light is reflected from the white sclera.

Drooping lid or ptosis may disturb development of binocularity and lead to amblyopia of the eye with ptosis. Therefore ptosis needs to be evaluated early in infancy. If the drooping lid does not cover the centre of the pupil, the optical axis, the risk of amblyopia is small during the first few months of life before the infant learns to sit.
In this case you can see the reflex of the flash in both pupil areas. It is not central in the right eye, which means that the eye was turning outwards. This infant was just about to fall asleep.

When the child starts to be upright, it is worthwhile to test now and then that the infant/child uses eyes equally, i.e. that covering the other eye that does not have ptosis does not disturb the infant more than covering of the eye with ptosis. The cover should only block the gaze, not touch the infant’s face.
When the child grows, ptosis may become less disturbing. Even then it is wise to follow the development of visual acuity at regular intervals either at home, if the parents can take care of the measurement, or at the basic health care or in an eye doctor’s office. In areas where there is shortage of the services of eye doctors, as many follow-up visits as possible should be arranged at the level of basic health care services or taken care by a nurse (or orthoptist if available) in the eye doctor’s office.

Until the age of three months most children have eyes turning in or out for brief periods, which is normal. A constant turn of an eye or restricted movements of an eye are always an abnormal finding and the infant needs to be examined by an ophthalmologist.
After the age of six months squint, strabismus, especially inward squint, should not occur more than briefly when the child is tired, or the outward squint when the child is thinking on something, not looking at anything and the eyes turn in their sleep position (s.c. Bell’s phenomenon, eyes turning out and up during sleep, which prevents corneas from drying if the lids are slightly open).
In many cases the cause of an inward turn of an eye is hyperopia, long sightedness. Proper corrective glasses straighten the eyes and development of vision can continue normally. Early detection of strabismus and support of normal development by glasses and follow-up of the development have decreased need of surgery in several countries.
In the lower picture the reflexes of the flash can be seen in the centre of the pupil in the right eye and at the edge of the pupil in the left eye. When the angle of squint is so large as in this case, the position of light reflexes (=Hirschberg test) is easy to record.

Pseudostrabismus is the most common false diagnosis related to vision development at the level of basic health care. If there are nasal folds covering the inner part of the sclera in both eyes, the child may seem to have esotropia, inward squint. Especially, when the head is slightly turned (to the right in this case), the eye seems to be squinting inward. However, it is better that a few children without strabismus are referred than that even one child with this treatable condition is not examined by an ophthalmologist.

Toward the end of the first year infants start to recognise family members by their faces and by their voices, if vision and hearing are normal. If an infant does not respond to family members differently from responds to strangers but does recognise their voices at the age of 10-11 months at the latest, vision needs to be carefully assessed. The infant may have large refractive errors or other causes that decrease image quality so that faces are not perceived well enough or there is a specific loss of face recognition. The faces are not perceived and recognised because the specific brain function has not developed.
Eye-hand coordination may not develop as expected. In a normally developing infant it starts as watching the hands and bringing them to the midline and into the mouth. Then the infant starts to hit hanging toys, which develops to grasping objects and exploring them with hands and mouth. At the age of six months many infants have a nearly compulsive desire to grasp everything within reach and hold it tight.
In these two important areas of development, deviations from normal age appropriate behaviours are common in children with brain damage related vision loss.
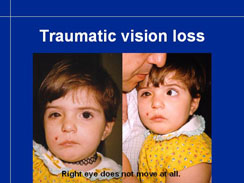
Accidents, especially traffic accidents, may cause loss of vision because of damage to the eye or optic nerve or because of brain damage. In this case there is right sided paresis of facial nerve, blind, non-moving right eye and deafness of the right ear. It will be possible to investigate first later when the child grows, whether there will be functional changes related to brain damage.

Accidents, especially traffic accidents, may cause loss of vision because of damage to the eye or optic nerve or because of brain damage. In this case there is right sided paresis of facial nerve, blind, non-moving right eye and deafness of the right ear. It will be possible to investigate first later when the child grows, whether there will be functional changes related to brain damage.

This slide summarises the most common deviations that should be detected during the first year of life so that the infant is treated and has adequate early intervention.
- shadow in red reflex, cataract, cloudy cornea, cloudy vitreous – at birth, at each visit
- delay in eye contact & early interaction
- unequal size of the eyes – glaucoma;
- ptosis
- strabismus, eyes should be aligned at 6 months, intermittent brief squint (when tired) tolerated
- infant does not recognize family members by face but does recognize them by voice –specific loss of face recognition or poor quality of image
- any other delay in visual cognitive development

Vision screening is best organised as a part of the basic health care, not as specific separate activities. The key persons in screening are health care centres in countries with national health care, in other countries doctors, general practitioners and paediatricians and the nurses working with the doctors or as independent health care practitioners. Many children, who have brain damage related vision loss, have strabismus and are therefore referred to ophthalmologists. If the infant has normal eyes, it is often forgotten to evaluate, whether the infant might also have brain damage related vision loss (CVI). At the hospital level orthoptists and strabismologistsare the key workers in the early diagnosis of CVI. Similarly, doctors taking care of infants with ROPshould know that there is an increased risk of brain damage and vision loss in these infants.
If an infant has an anterior visual impairment, it does not prevent the infant from having also brain damage.

In preschool years, general vision screening based on measurement of visual acuity is most usual at the age of four years because at that age nearly all normally/ typically developing children can be tested during the first examination. If there are worries about the visual acuity, most children can be tested with single symbol LEA tests before the age of two years and soon after that age also with the screening line tests.
Children who ”do not co-operate” or “have short attention span” should be tested twice and if their testability does not become normal, they need to be referred. It is important to rule out that their poor functioning in the test situation is not caused by poor vision. If their vision is found normal they need to be referred to a paediatric neurologist.
Children with intellectual disabilities are likely to fail the screening examination and need to be examined by an ophthalmologist even if they have been examined by an ophthalmologist as an infant. Likewise children with motor problems and children with hearing problems need to be referred. There is no screening method that would cover all the aspects needed for detection of children with vision problems in these groups of children with special needs. CONE Adaptation test can be used in health examination of hearing impaired children to detect retinitis pigmentosa early, which is important for the planning of special education.

In the vision screening at preschool age, at 4 years and at kindergarten and during the 1st or 2nd grade, amblyopia is the main finding in many countries, although it should have been treated by then, but also large refractive errors and children with visual impairment may be detected. New cases of visual impairment are usually children with retinal degenerations with normal looking eyes. Brain damage related vision loss may not cause changes in visual acuity and therefore all common symptoms of CVI should be included in the questionnaire used in the examination of development at the school. When the children grow, more subtle deviations from normal visual functioning can become noticeable. Teachers are usually not well aware of cognitive vision losses, which may cause misunderstandings and major difficulties in learning, if not recognised and compensated with special education.
Children with other impairments need to have their vision examined by an ophthalmologist who is accustomed to assess handicapped children and works in the local rehabilitation team. Many children need to have the test situations trained as a part of teaching in kindergarten and at school so that their visual functioning can be assessed.

In vision screening we need to decide which tests are used, need to know what they measure and which other observations need to be made. We also need to decide the pass/fail criteria. Often it is wise to allow the screeners to refer those few children, of whom they feel that there might be something wrong with the child (“gut feeling”), even if the child passed the screening tests.

Visual acuity measurement is the most often used test in vision screening in preschool and in school age. In infancy visual acuity can be measured only as response to gratings, which is not used in vision screening.
Visual acuity can be measured with optotype tests when the child can match the test symbols. With LEA SYMBOLS® it is possible to train an infant to match them soon after the first birthday. After training with the LEA 3D Puzzle the measurement of binocular visual acuity has been possible at the age of thirteen months in a few infants and more often after the age of 18 months.
By bringing the distance test with 30M optotypes to 30 cm (one foot) distance, it is possible to measure visual acuity values to 0.01 (6/600, 20/2000) and by bringing it still closer, even lower than that. If the largest symbols cannot be recognized at the closest distances, there is no form perception. Then visual acuity can be “detection of hand movements” or only “perception of light” with or without projection, i.e. awareness in which direction the light source is. (Counting fingers is an inadequate way of reporting sharpness of vision because fingers are not calibrated and the background against which the fingers are shown is not a standard surface.)

In Nordic countries we have used a collection of small items to assess detection of small objects. In this slide we see Sheridan balls and toys, colourful small balls, Muumintroll figures and soft sweets of 12 different sizes. (Black-and-white copy of this slide was used in the textbook “Assessment of Vision in Children” by Hyvärinen and Lindstedt, 1981).
Cover test (shown in the next slide) is used in many countries to detect small angle strabismus and differences in the central vision between the eyes. When an eye is covered, the tester observes what happens to the uncovered eye. If the uncovered eye was not looking at the picture on the fixation stick, it will move to fixate the target, i.e. there is a corrective movement.
When the strabismic eye is covered, there is no movement in the leading eye.
If the strabismic eye has developed an eccentric fixation, it may not move during cover test but a slight difference in the position of the light reflexes (Hirschberg test) may be present. These small angle squints are so difficult to detect that often the condition is diagnosed first when visual acuity can be carefully measured until threshold (until the smallest line read correctly).
If there seems to be a small angle squint in a toddler, it is worthwhile to teach the child to function in the test situation before trying to test visual acuity. A difference in visual acuity values can often be measured at the age of two years with line tests if the child has trained at home.

This child has esotropia, inward squint, but uses both eyes equally well, which is called alternating esotropia. When the fixating eye is coved, the squinting eye fixates steadily on the fixation target and remains fixating when the cover is removed. Cover needs to be held in front of the fixating eye until the squinting eye has fixated the target. Again enough time needs to be given to observe that the previously squinting eye keeps fixation when the cover is removed from front of the other eye. These children need to be referred so that their refractive errors will be measured and the possibility of treatment with glasses and/or operation is considered.

Lang stereo test is used in some countries as an adjunct to visual acuity measurements. As long as the child cannot tell which pictures there are, the response is difficult to assess. An obvious, stable fixation at the pictures and shift from one to the other and back can be observed as early as at the age of four and half months in visually alert infants.

Vision screening at the age of four years is designed for detection of amblyopia. The target population of amblyopia screening are symptom free children. If a child has symptoms of any kind (strabismus, squeezing eyes during testing, head tilt or turn, itchy or red eyes etc.), (s)he is referred for treatment independent of visual acuity values.
Visual acuity can be measured with single symbols quite early, the earliest at the age of 13-16 months. Single symbols do not detect amblyopia as well as line tests but large differences in visual acuity between the eyes can be detected.

Training with the 3D Puzzle helps the child to develop the concept same/different first between colours, then between black-and-white concrete forms, then making the big step comparing 3D forms and flat pictures.

Training is especially important in testing children with delays in development. Information for Parents ->Training for vision testing

Screening visual acuity tests are easier than the standard line tests. The lines are further apart and the grey surface decreases dazzle in photophobic children. This type of test is faster than the standard test and easier for the tester and the child to know on which line to read.

Children answer either by matching or naming (using spoken words or signs). For detailed instructions see:
http://www.lea-test.fi/en/vistests/instruct/2520-99/index.html

The smaller lines are on the reverse side of the test until 1.25 (6/5, 20/16) line.

After measurement of the binocular near vision acuity, the child is shown the distance screener and told that the same pictures will be shown at a greater distance. Binocular and monocular values are measured. If covering of the left eye (which is usually covered first) causes a strong negative reaction, cover the right eye first.
It is important to keep in mind that skipping symbols is a feature typical to amblyopic eyes. Even if the visual acuity difference is less than two lines between the eyes, it may be an important finding. If one notices that the child has motor difficulties, like skipping symbols, the tester should be alerted to the possibility that the child might have beginning mild amblyopia developing in an eye or has undiagnosed brain damage.

Covering is easiest with this special “Screening frame” that can be used to cover both eyes in turn. It is easy to wipe clean and can be used for years. The screening frame comes in two sizes and in several colours, of which the dark purple seems to be the favourite of many children. It blocks the vision of the covered eye more completely than the white one, which lets some diffuse light through it.

In the distance screener there is only one line on each page to make it easier for the child to know where to read. If however, the child makes an error and starts to read the line a second time, there is another page with the same size of optotypes for this situation. In screening a line should be read only once. The tester may say to the child “Let’s take another line of similar pictures so you read it without hurrying.”

This publication by World Health Organisation, WHO/PBL/03.91, was published in August 2004 and describes the recommended routine in measurement of visual acuity in population-based surveys, and thus applies also to paediatric vision screening.
For details see http://whqlibdoc.who.int/hq/2003/WHO_PBL_03.91.pdf
One of the most important recommendations is measurement of visual acuity at near. It recognises the importance of near vision in all functioning. Measurement of near vision with optotype tests is not common in all countries but is warmly recommended, because with this simple measurement at near we can diagnose that a low visual acuity at distance is related to myopia, the child has normal visual acuity and does not need to be referred, which means a great saving for the services and also for the parents, if they must travel a long distance to (their) an ophthalmologist.

The central features of the WHO document are:

Small lightboxes solve the problem of standard illumination. The present generation of lightboxes uses diodes instead of a lamp. Therefore they have stable luminance and tolerate traveling. The slide shows the technique of covering the line above the line to be read. The end of the cover is slid between the test and the frame of the lightbox, which helps in keeping it horizontal.

To summarise the visual acuity screening: the word “binocular” is used here to mean ‘both eyes open’
The pass/fail limit has been 0.5 (6/12, 20/40) binocularly at distance and near and less than two lines difference between the eyes at distance and near, when visual acuity was measured until threshold. Clark et al study showed that if the visual acuity of the worse eye was 0.5 (6/12) or better and that of the leading eye 1.0 (6/6) or better, there was no statistical difference in the results of treatment when the treatment was started at the age of four years compared with results of treatment that was started at the age of five years. This can be interpreted so that glasses and training may be postponed by a year in this group of children with mild amblyopia, if treatment is found problematic. The study did not include children with visual acuity less than 0.16 (6/36) in the amblyopic eye. In the group of children with visual acuity 0.16 – 0.3 (20/125 – 20/63; 6/36 – 6/18) in the amblyopic eye, full treatment showed substantial effect. The results thus show, that the delay in treatment is justifiable only in the mildest cases of amblyopia. However, the more severe cases need to be treated and thus screening should be at four rather than at five years of age.
In many cases, when the difference between the two eyes is two whole lines, there is no real amblyopia or it is very mild, because the difference in visual acuity values disappears when the child is tested with proper refractive correction or (s)he has had glasses for less than a month. Therefore visual acuity values should be measured with optimal correction after the cycloplegic measurement of refractive errors. Optimal correction is not equal to full correction in most cases.

With the tests there are detailed instructions and the same instructions are on the homepage www.lea-test.fi
The important details are:
- Decide with the child the mode of answering: matching or naming, any names are OK. To decrease the time used for testing, ask only the first optotype on each line or each second line until the child hesitates or answers incorrectly. Go up one line and ask the child to read all optotypes on that line. (This allows the child to focus carefully, after which up to two more lines may be read correctly.)
- Continue until threshold, i.e. at least three out of five optotypes are read correctly. If only two out of five are read correctly, record the result: visual acuity of the previous line (+2).

Visual acuity based screening is designed to detect amblyopia in healthy children. It detects also a few cases of high refractive errors and an even smaller number of children with visual impairment.
It is unlikely to detect visually impaired children with brain damage related vision loss, if their visual acuity values are normal. Therefore the nursery school and kindergarten teachers should have training in observing strategies and behaviours typical to vision loss due to “hidden” brain damage.
If there is a larger than usual difference between visual acuity at distance and visual acuity at near, it is worth-while to measure visual acuity values with the more crowded near test to find out, whether there is increased crowding.
If there are any of the typical features of cognitive vision loss (pdf), the child is referred to thorough ophthalmologic and neurological assessments. The earlier we find processing problems (CVI), the more time there is to find compensatory strategies before the school age. Cognitive vision loss is often more problematic in integrated education than vision loss caused by lesions in the eyes and/or optic pathways that affect image quality. Processing problems cannot be demonstrated with demonstration glasses that can approximately depict the nature of poor image quality (Part I/ Demonstration glasses).
In vision screening there are seldom children with undiagnosed visual impairment, most cases have been found (should have been found) in infancy, if present from birth. Some inherited disorders manifest themselves between four and ten years of age, so age normal visual acuity values do not guarantee that the child has normal vision. The age norm is low, 0.5 with both eyes open. Many normally sighted children read 1.25 (6/5, 20/16) line at the age of four years.
Because the visual acuity screening is only screening, it is not wise to predict any forms of treatment based on the results of screening. Need of treatment is evaluated after thorough clinical assessment of the child’s vision.

Children with intellectual disabilities (ID) are assessed by an ophthalmologist at the time of the diagnosis of ID or at the age of 3-4 months to diagnose refractive errors and weak accommodation. The follow-up of infants and children with Down syndrome is the same as that of their peers.
At the age of four years some of the best functioning children with developmental delays can be tested with the routine screening tests. It is good to try to test all children with ID to collect information for planning of special education. These children need to be examined by an ophthalmologist because they are likely to have problems more often than children with normal development of intellectual functions. Cataracts may develop in preschool and school age, squint is common and processing problems are difficult to diagnose because of communication problems. Among the children with severe intellectual disability at least half of the children have vision problems that need to be treated because the disorders disturb learning.
It is good to check that the glasses are of good quality. Unfortunately, these children often have glasses that glide along the nose so the child looks over the glasses much of the time. Bifocal glasses may have too small and too low placed near corrections, which cannot be properly used by the child. (Such glasses I do not call ‘eye glasses’ but ‘cheek glasses’.)

Emmetropisation of refractive errors, which means decrease in the size of refractive errors, is a typical feature in the development of normal children. Young children are more far sighted than school children. This shift in the refractive power is not common among children with Down syndrome. (This slide is based on two slides of Margaret Woodhouse)
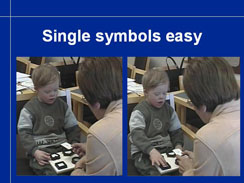

At the age of four years many children with ID can be tested with single symbols but testing with line tests takes time and children easily lose their motivation.

Single symbol tests must often be used still on the 2nd grade, in some cases through the school age, if a child can handle pictures of concrete objects (optotypes of LEA tests) but not pictures of such abstract symbols as numbers and letters.

Transdisciplinary assessment seems to be the strategy that works best in the assessment of visual functioning of children with delays in development. Transdisciplinary means closer collaboration than interdisciplinary. The team members know the most important test situations and are able to use the tests as a part of daily activities and classroom work. The test situations need to be repeated with regular intervals because a child may have been tired, hungry or nervous when assessed in the doctor’s office. On the other hand, the test situation in the doctor’s office may have been calm and relaxed and the measured values good when there were no distracting factors. The child may not be able to function at the same level in an integrated school situation with visual and auditory noise around.

This is a typical transdisciplinary test situation. Communication is led by the teacher who knows the support signs and dialect of the child, the ophthalmologist is out of the sight of the child and only changes the test cards without saying anything. Observation of the child’s behaviour is easier when someone else is in charge of the communication. Most people can either communicate well, be absorbed in the interaction with the child or they can observe well, very few people can perform in both activities simultaneously. – Note, that the child uses the sign “good” when she is able to match the picture on the card with the similar 3D puzzle piece.

In school age a child’s assistant is often the person who can keep the child’s concentration in the tasks related to testing: not through a normal test, but at least during two or three answers.

In vision screening at school, number or letter charts are used in the Western world. The Roman letter charts do not function in countries where other characters are used. Therefore numbers are a more suitable set of optotypes in comparative studies of visual functioning covering several cultures. Like the LEA SYMBOLS®, also LEA NUMBERS® have been calibrated against the Landolt C, the international reference optotype since 1988.

Vision screening at school-age is different from vision screening in the preschool. Amblyopia should have been diagnosed and treated before school age, new cases of vision loss are rare, so the goal of vision screening is to find the children who have not noticed that they have difficulties in classroom work because of blurred images. There is no general pass/fail level in visual acuity values because the school situations vary so much. A small myopic child who can sit in the front row may have no problems in classroom work before his/her binocular visual acuity is 0.2 – 0.3( 6/30 – 6/20; 20/100 – 20/60), whereas a tall child may need glasses when binocular visual acuity is 0.8 (6/9 – 20/60), if (s)he must sit in the back of the classroom and teacher’s handwriting and projected texts are small.

Children with severe motor problems need to be assessed at school, where their physiotherapists can support the children during testing. If a child cannot talk, gaze pointing may be used in matching. A child may also be able to point with foot or by turning head toward the correct answer of two choices. Severely impaired children cannot be screened like their normally functioning peers. Instead they are always assessed when other children are screened. Special education requires also ‘special screening’ and special assessment. Special screening is for example testing for visual adaptation to lower luminance at schools for the deaf children, because retinal disorders are common and not otherwise noticeable during the first years at school.

As a summary:
Vision screening to detect visual impairment is a small but important part of general vision screening to detect amblyopia or risks to develop amblyopia and large refractive errors. “Screening of children with special needs” means thorough ophthalmologic assessment of each child with a disorder that causes a high risk of impaired vision, training of children for testing and good transdisciplinary efforts with day care, nursery schools, kindergartens and grade schools.

Since more than 60% per cent of children with impaired vision have other impairments, detection of visual impairment among children known to have other impairments is the most effective way of detecting visual impairment and large refractive errors early. These children are usually in intensive medical care during the first year of life. Thus it is not difficult to arrange that each child is thoroughly assessed. When early diagnosis is a part of basic paediatric care, it does not cause economic problems and it improves the care of the child and planning of special education.
