Assessment of Visual Functioning
of Disabled Infants and Children
as
Transdisciplinary Team Work
Slide 18.
Before the assessment of visual functioning or “functional vision”, following information should be available from the clinical examinations of vision:
- structure of the eyes
- structure of the visual pathways
- refractive errors
- spectacles, under- or overcorrections
- ocular motor functions
- accommodation, convergence and pupil reactions
The basic visual functions are assessed and reported by ophthalmologists and optometrists. The infant should have proper glasses fitted by an optometrist, not too small or too large, not gliding along the nose and the infant should be accustomed to use the glasses at least a few days, preferably a few months, before the educational assessment of visual functioning.
Slide 19.
In the age appropriate assessment we use the normal development of vision as a guide:
Most visually impaired infants have other impairments that affect the development of vision and communication. Therefore there can be delays in:
- eye contact
- social smile
- noticing own hands and exploring them
- keen observation of movements of lips of adults
- bringing hands to midline and into mouth
- copying of goal-directed hand movements of other children
- between 7 and 10 months recognition of family members by facial features before they say something. If any function is delayed, the infant needs to be referred for consultation.
It is advisable to record when each of these functions can be observed and whether these functions appeared age appropriately or at the same age as in the other children of the family. Individual variation in each area of development is wide, up to months and is related to the experiences of the infant. For example, some infants start to point with finger at the age of 20 weeks since they saw finger pointing daily in different activities; other infants have grown unusually dexterous in building towers with small cubes because the older siblings demonstrated their skills in building with blocks as soon as the infant learned to sit.
Other functions related to mirror neuron system and development of anticipation of daily activities and movement patterns are observed or discussed with the infant’s therapist and mother, for example when watching the reciprocal movements of the mother and baby during baby massage (See the LEO video). At the age of 5 to 7 months most infants respond when they see mother taking a baby food jar or another object that signals important activity.
Slide 20.


Infants’ motor activities are fun to observe if a group of infants of about the same age can participate in activities where they can observe other infants’ motor functions and copy them.
Pictures in Figure 20 are from the Art Museum in Pori, Finland where young artists are given opportunity to express themselves. Also visually impaired infants with some sight enjoy this play situation.
Hands are the second eyes of visually impaired infants and should become well trained in exploring the home. For fine details visually impaired children use the tip of the tongue and lips. Mouthing is a practical strategy, not an “autistic behavior” in infants and children with severe vision loss. After mouthing the child should be helped to explore the surface also with fingertips to compare how it feels when using these two different strategies. Verbal description of exploration during play is important and helps parents and therapist to become aware of hyper- or hyposensitivity of hands or only some fingers or feet and toes.
Slide 21.



If an infant is hypotonic and has not fixated or followed visual targets, the stimulus should be large, with stripes and face on it (as in this first LEA-doll) to activate ocular motor functions and head control. At the time of this infant’s visit in my office we were testing a prototype of a large light box that could combine high contrast visuotactile toys and visuotactile pictures. The infant who did not have head control when coming in, held his head up for several minutes to see the picture in front of him. Visual information, especially picture of face is a powerful activator of motor functions.
Slide 22 and 23.



When an infant has stayed several weeks or months in the hospital, like the baby in these pictures, many developmental milestones may not have been reached. The infant might have very limited attentional fields and no interest in using vision. These infants have often had negative experiences of unknown persons coming close; a new voice has meant a new type of pain. Therefore when assessing an infant for the first time it is wise to let the person of the early intervention team who has already met the infant to start the communication. In the above case it was infant’s own physiotherapist. She was asked to move the illuminated ball (the ‘instrument’ is a ball for kittens with rough surface and small holes, through which the penlight was pushed in the ball) from the periphery of the visual field to the midline on both sides. As you can see in the video recording, the infant responded only at the midline.
If an infant is unable to shift attention from the midline, the hands of the infant can be used as stimuli. They are placed, one at a time on the illuminated ball, which should have uneven surface. Baby’s fingers form a grating-like pattern against the ball and are simultaneously feeling the surface of the ball as tactile information, the form as haptic information and the movements of the arm and hand. This kind of multimodal stimulus is easy to include in the assessment situation. It often motivates the infant to become an active part of the assessment. It is also good training of the therapists for including activation of vision as an integral part of physiotherapy and occupational therapy.
Since most visually impaired infants have other impairments that require therapies from early on, it is important that all therapists learn to consult vision team for new tips and information on infant’s vision, and to make sure that they will receive further information when the infant will have follow-up assessments of visual functioning.
Slide 24 and 25.



If the infant responds to near correction glasses with a brief eye contact (Slide 24), test glasses can be given on loan until the infant’s own glasses are made in a comfortable, well-fitted frame. Picture in the middle is from a video taken 10 weeks after the previous one. The infant had developed good communication with her therapist and used both hands in the midline playing with plastic beads, her favorite toy. - Visual and motor training can be combined in many ways. A favorite toy often entices an infant to perform a demanding motor function for the first time; in this case turning from back to stomach. – A few weeks later the right eyes responses to gratings lagged those of the left eye. Therefore the left eye was patched during physiotherapy while the infant was training her weaker right hand to grasp while seated. The colorful high contrast toy in her hand was an effective stimulus for the right eye. The goal of the physiotherapeutic training was to entice the infant to start turning head when sitting. Visually activating toys helped also in this situation.
The structures in the environment should be explored with all senses to support the limited visual information. Playmat can be made so that the boarder in colours coincides with the surface quality of the materials: dark colours are smooth, light colours are rough. The two ends of the playmat are clearly different. - Resonance board activates moving because the child gets auditory information on his movements. Surfaces like a metal washing basin and plastic waste basket give different echoes and create an interesting auditory play area for listening skills. - “Little room” can be really little if the infant is a tiny prematurely born child, a shoe or boot box serves well in the beginning, later usual brown boxes of increasing size. The box should be so little that the infant can easily reach to the walls that are decorated with varying materials from the household.
Slide 26.


The commercially available “little room” is meant for school age children at early developmental level. The transparent ceiling makes observation of blind children easy but a child with impaired but useful vision should have a non-translucent ceiling to experience the space as a closed space with both vision and hearing. If the box is supported with a light wooden frame, it is easy to move for the infant to the room where the mother or other person is working and cannot carry the infant in sling during the work. If a thick rubber band is tied on the frame and hangs in the upper part of the little room so that toys tied to it are within the reach of the infant, he can explore the toys with hands, pull them down to explore them with his mouth and when he lets them go, they do not disappear but are to be found in the same place as before. This facilitates the development of object permanence, which often shows delays if toys fallen from the hand of a visually impaired infant/child are given back to the child.
Slide 27.
The short list in Slide 27 summarizes the most important developmental areas that should be observed and supported in the early intervention. Since young visually impaired infants often lay inactive and listen if left in the crib or on the floor, they should be as much as possible with the mother in a sling where they experience movement patterns, communication and are close to all activities of the home. Development of movements requires baby gymnastics and massage as a brief part of many activities during the day. The training by a therapist one hour two or three times a week is far too little and therefore the parents should learn to repeat the activities learned in the therapies several times each day. When the infant is becoming too heavy to carry, he usually can sit in a high chair where he can better see what the mother is doing in the kitchen. As soon as the infant can move along furniture he should be allowed to “help” in all activities to learn what the different sounds and noises mean.
These few pictures are from the video ”Leo learns by doing” (Good-Lite, Chicago, Ill.) that depicts how motor activities can be included in play situations of a nearly blind infant, daily activities at home and recreation, like baby swimming. Similar activities can be recommended for all infants.
Slide 29.
Vision loss is gradual in several common eye diseases like macular dystrophies and retinitis pigmentosa. As in early visual loss, collaboration between diagnostic and early intervention services should be good. There are still hospitals where children are not referred to rehabilitation services until their visual acuity is less than 6/18 (20/60, 0.3). This visual acuity value is related to reporting to international registration. Rehabilitation as early intervention should also in slowly progressive disorders start at the time of first diagnosis of vision loss, i.e. before the diagnosis is confirmed, which may take months. During the diagnostic work-up it is possible to arrange so that an older child with the same or closely similar diagnosis will be with his parent in the waiting room at the same time as the new child. The early intervention worker can discuss with this known family briefly, after which it is easier to introduce her to the new family as the person who is in charge of the questions related to social services, kindergarten, school and recreational activities. Sometimes it is a good idea to have several children with similar vision loss visiting the eye clinic and inform all families on current interesting questions, presently about gene therapies. Children learn to know each other and can have contact via phone and e-mail already before they have participated in recreational camps and other activities for children with impaired vision and other limited functions.
If early intervention and rehabilitation for visually impaired children are not started as a function of a worker of the low vision clinic in the hospital, the connection between the hospital and the rehabilitation services should be active. This is especially important in case of dual sensory disorder because the future communication should be considered by people who know this rare combination of functional losses. Since in near future it might be possible of treat some types of retinal disorders, all clinical measurements should be rigorously standardized so that even small changes can be recorded. In Northern countries exposure to day light varies a lot and therefore there should be a standard period before tests at a certain luminance level using the usual refractive and filter correction. We should develop a routine set of tests and their order to make comparative studies possible. Functions like contrast sensitivity should be assessed using optotype and grating tests to follow whether the declination of the slope changes the same way in the small central and larger areas of the visual field. It looks like that the first improvement happens in motion perception at low frequencies in the periphery of the visual field. Therefore standardized measurements using also large enough stimuli should be agreed upon. The small 4 degree stimuli that are used in studies of normal functions of the retina result in misleading findings in retinal degenerations. This discussion was not a part of the lecture in Montreal but was discussed later and is added here because it was specifically asked for discussion after the lecture.
Testing Vision
Testing vision of children with different impairments differs from testing vision in usual vision screening. We try to start the measurements with optotype tests as early as possible. That requires the concept of “same”, which can be learned first comparing colours, later forms. These features are combined in the LEA Puzzle that infants can start using already before their first birthday. Some infants have started as early as at the age of 10 months but at that age they make noises with puzzle pieces and bite them. At the age of 18 to 24 months children can play with the colorful and the black-and-white side of the puzzle, after which they learn to place the puzzle pieces on cards with large pictures of the optotypes, then smaller pictures and finally even the smallest pictures of the Playing Cards test. Other children prefer placing the Playing Cards on the Puzzle board.
Slide 31.




Note the position of the hand when the child is about to grasp the black-and-white puzzle piece “house”. Hand has turned to grasp the bottom of the house so that the puzzle piece can be turned and placed in its cut-out. The child has the concept of orientation in space and can use it in her eye-hand coordination.
The Puzzle is an educational toy and at the same time a neuropsychological test revealing awareness of orientation of objects and using that information in hand functions, eye-hand coordination. If the puzzle board is turned 90 degrees while turning the black &white side up, we can observe child’s short time memory for localization: the child starts to put the puzzle piece in its earlier place, stops in mid-air and then puts it in the correct cut-out.
Slide 32.




More than half of all visually impaired children have at least one other impairment; among children with intellectual disability visual impairment varies from 30 to 90 per cent depending on the severity of brain damage. These children can be examined several years earlier if they play with the LEA Puzzle in their nursery school or at home, sometimes only for a few weeks.
Slide 33.


Person with best communication with the infant or child should be used while training for testing and also in the test situation. The ophthalmologist or optometrist can be present and watch that the test is correctly performed. Note at the end of the video the girl signing “I’m good”. She has normal hearing but had some speech delay and therefore used sign language. – In the assessment of school children with special needs we often use a special teacher as the tester and the child’s classroom assistant as the support person in the training for testing of visual acuity.
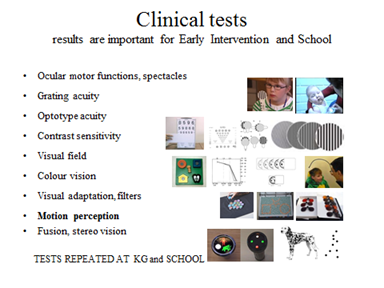
Slide 34.
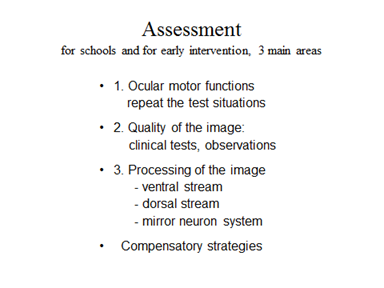
Assessment for early intervention or for school has three main parts: assessment of ocular motor functions, quality of the visual information entering the brain, and visual processing functions. If the teacher(s) have sent a list of their problems to the hospital, they can get quite useful information in the report from the ophthalmologist and the optometrist who have planned the glasses and chosen the devices. Unfortunately, the report from ophthalmologist can be a copy of the ophthalmologist’s notes that can be difficult to decipher and may not give enough information for repetition of the test situations and understanding the child’s problems.
The persons in the educational assessment team vary a lot. Ideally there is a special itinerary teacher from the School for the Blind and Visually Impaired who is trained in educational assessment of different visually impaired children and/or a pediatric rehabilitation optometrist helping the teachers, therapists and the school nurse in the assessment. Ideally there is also clear information from the hospital because it is the foundation on which the educational assessment is built.
Educational assessments have become much more difficult than before because severely visually impaired children with other impairments are integrated in local schools. Some of these children have both anterior, ocular impairment and posterior, brain damage related changes in vision, some have only scattered cortical and subcortical changes with normal routine clinical findings. In this situation doctors in the hospital have difficulties in assessing the visual functioning if they do not have thorough, well-structured information about the problems at the school. At the same time teachers and therapists do not understand the results of the clinical vision tests and neurological examinations if they have not been present in the examination or learned about the tests so that they can repeat the tests at school where the results are usually better than in the doctor’s office.
The solution of this difficult situation is in improving the communication between hospitals and schools, especially in improving the information from schools to hospitals so that doctors can develop their assessment and the language of their reports. The classroom teachers and assistants need further education to understand their students’ complex situations and to be able to follow the individual learning plans. This last requirement is often forgotten when placing a child in a school where there has never been a visually impaired child before or even if there was one before, the disorder and condition of the student were different and thus also the learning strategies quite different. Understanding the visually impaired child’s way of learning requires basic understanding of many atypical brain functions and their effects on learning and teaching. The information for this understanding should be created in the medical and educational assessments.
Slide 35.
Ocular motor functions are usually well described so the team only compares whether they can see the functions as these are described in the report. The most important functions are: 1) Fixation on penlight compared with fixation on details of a small picture: does the fixation change from the usually central fixation to the light to eccentric fixation to look carefully at details? (Video in slide 35 B) 2) Saccades, both short and long saccades from object to object and during reading. 3) Convergence – divergence and pupil reaction during convergence. If accommodation has not been measured at the hospital, the rehab optometrist can measure it. Otherwise it is possible to 4) later compare distance and near visual acuity values and if the near acuity value is lower than the distance acuity value, to test whether near correction improves it.
Distance and near visual acuity testing for vision screening is routinely used at Kindergarten and schools in some countries, in other countries only distance visual acuity. In the assessment of visual functioning of children with impaired vision and other impairments we need to use many more tests to know or estimate what kind visual image the child uses for processing functions.
If the teachers and therapists have assessed the functions of a child, they can inform the hospital in which functions they feel vision is not used the way a typical child uses his vision. It is important to describe in detail the observations that make them suspect deviation from norm in the use of vision. Based on these questions from school, ophthalmologist and neurologist can use additional tests and investigations to answer, whether it is 1) blurred or distorted image or 2) changes in cortical functions or 3) both that is the cause of the unusual behaviors or 4) something quite different is likely to be the cause. Repeating at least some of the clinical measurements at school helps to understand what kind of losses there are in visual functioning.
In testing with visual acuity tests we often measure first with the calibrated LEA SYMBOLS® (which are pictures of concrete objects) and LEA NUMBERS® tests and then Sloan letter tests for distance and near and, when needed also with single and line tests to document possible differences in perception and recognition between pictures of concrete objects and abstract letters and numbers. Letters cannot be calibrated with Landolt C so that they would be equally recognizable but if Sloan letters are correctly chosen for each line the difference in VA values compared with Landolt C and LEA tests is less than half a line in the means of large groups of normally sighted children. Since there is often variation in the recognition functions of children with brain damage, visual acuity values with different tests may reveal some of these variations. Many children with developmental delays cannot be tested with abstract forms, Landolt C, letters and numbers, only with the LEA SYMBOLS®.
The relationship between optotype acuity and grating acuity shows large variation in children with atypical visual development. It is possible that visual acuity value is 6/1500 and grating acuity is 4 cpd, i.e. thirty times better than the optotype acuity value (if 30 cpd is assumed to be equal to 6/6, 20/20, 1.0 optotype acuity - see the lecture on visual acuity tests). On the other hand optotype acuity value can be 6/6 or 6/5 and grating acuity 4 cpd, one eight of the optotype acuity value. We do not always know the causes of the differences but the problems often seem to be related to the early visual processing in the occipital lobe.
Contrast sensitivity measurements are equally complex and should also be measured with optotype and grating tests. Some children cannot be tested with other than detection tests, i.e. Teller Acuity Cards or LEA GRATINGS at full contrast and with Cambridge Low Contrast Gratings at low contrast levels. Whenever gratings are used, it is important to test whether the lines are seen straight or as irregular network. If fine lines are not seen as straight lines but as a distorted network, the students cannot use diagrams based on fine lines independent of VA values nor can they cut along threads because they do not perceive them.
If contrast sensitivity is low, color vision cannot be tested with screening tests because they are low contrast tests. Panel 16 with its large caps is easier than Farnsworth D-15. The colours of these two tests are equal, of the same Munsell papers.
In measurement of visual field we can use finger perimetry, interesting objects or Flicker Wand to document the size of the visual field. Since many children have difficulties in shifting attention, the measurement of visual field is more reliable when the response is a reflex saccade to the stimulus coming from behind the child. When the visual fields are measured at the hospital it would be good to also measure the difference between the visual field based of reflex saccades and that based on responding by pressing a key. If a child must concentrate on head and trunk control, it is usually impossible to attend to the fixation mark and notice the stimulus in the peripheral visual field. Variation in the size of attended visual field should be observed at school because there may have been situations that were impossible to create in the low vision clinic. At times some children may bump into objects and people as if they had complete hemianopia or neglect. Central small fields can be controlled using white paper with a hole in the middle where another person controls fixation, if needed, while the tester records the size of the visual field using dark pencil or dots as stimuli. If the distance from the eyes to the paper is 57 cm, then 1 cm on the paper is equal to 1 degree of visual angle.
For motion perception we have too few pediatric tests. Loss of motion perception at high speeds affects lip reading, gestures, traffic vision, and perception of movements in gymnastics and all group plays and games.
If at least two ophthalmologists of the Eye Hospital could visit the special schools when integrated students with impaired vision have their support periods, they would learn about the needs of teachers better. The fine details in reading and mathematics remain within the specialty of education when it comes to children who do not have visual memory; visual imagination or three dimensional concrete visual world or abstract space so that, for example, they cannot imagine the number line.
