0-3 months:
Severe vision impairment affects development of brain: if vision is not having its dominant place as the avenue of information, it does not get its normal representation in cortical functions but tactile and auditory information take over cell groups that normally combine information from vision and other modalities (for more details see the deprivation study)
The effect of severe vision impairment is first seen in oculomotor functions. Normal eye movements do not develop but the eyes have slow roving movements or nystagmus. Sometimes nystagmus is the more benign inherited motor nystagmus that may be related to mild or moderate vision impairment.
Inactivity is often a typical feature in the behaviour of a visually impaired baby. In a normal infant visual information functions as an activator of brain functions. When visual information flows into the brain, it is used for seeing but simultaneously it also activates the ascending reticular formation, a network of neurons, that then activates the brain cortex, which is called arousal.
When eyes are opened, visual information flows into the ascending reticular formation that in turn activates the brain cortex, causes arousal. The person wakes up.
If an infant is unaware of visual world around him/her, this unawareness affects the infant's wakefulness and motor functions. Often an infant is thought to be sleepy because it does not open the eyes; opening the eyes does not change the image so there is no reward. Some infants move very little, the usual reflexive movements are sparse because the infant is not stimulated by the environment.



This infant with opaque corneas was very poorly awake before an operation of the cornea resulted in clear central cornea for a few weeks. During these few weeks the baby quickly caught up the delays in motor development and studied everything within reach both visually and tactily.
Some newborn keep their head turned on the shoulder until they become aware of vision and their hands. This is sometimes misdiagnosed as torticollis. It disappears sooner if the physiotherapist uses high contrast objects or a lightbox to get the gaze moving to the midline of the body and repeatedly brings the hands to the midline.
Vision and motor development are closely related. When a normally sighted infant sees his/her hand and brings it into the mouth, the early asymmetric tonic neck reflex (ATNR) is counteracted. If a visually impaired infant does not see his/her hands there is no incentive to explore them with the mouth and the early reflex pattern remains. Therefore playing with the infants' hands, guiding them to meet in the midline and bringing them into the mouth are important moments in play therapy.
Infants who have loss of central vision due to retinal scars (toxoplasmosis) or due to damage to the visual pathways must use the part of visual field next to the edge of the central scotoma and seem to look past the person whom they look at and therefore do not have normal eye contact. In the beginning the area of retina used for fixation (PRL=preferred retinal locus) varies but then the infant may start using a certain area or may use different areas of the retina in different visual tasks.
Since we experience eye contact with a baby positive and important, loss of eye contact is emotionally difficult to the parents but also to other persons taking care of the baby. Abnormal eye contact needs to be discussed with the parents and care takers and early interaction supported by nonvisual communication and visual communication very close to the infant. Infants who are in incubators or need to be operated and after the operation stay in the intensive care units should be kept on the lap as soon and as often as possible. They are often so sleepy that their visual activation is not feasible. When they start to be awake simple pictures can be placed in the incubator or crib. When strong visual stimuli are introduced, infant needs to be carefully observed for increase in heart rate and breathing to make sure that the infant is not overstimulated. Inhibitory mechanisms are not well developed in young infants so signs of too strong stimulation need to be watched.

Simple geometric forms with good contrast interest the very young infants. If the pictures are made of plastic they are easy to wipe clean. Since tiny infants do not touch them they last for years in good condition.
| Video 1 | Video 2, 3 & 4 | |

|

|
When playing with a young, severely ill infant one needs to watch signs of overstimulation. This nearly blind infant with ROP (retinopathy of prematurity) and hydrocephalus becomes active during play therapy where lightbox and simple high contrast toys are used under guidance of an experienced NDT therapist.
In the video you see that the infant's hands are brought to the midline. This helps many infants to bring the eyes to the midline and to look at the person in front of them. Note how close the playthings are presented to a severely visually impaired child. The responses to visual stimulation are weak but present and the infant clearly enjoys the play situation. During the usual clinical examination this infant did not respond to any of the diagnostic toys.
Eye movements, quick saccades and slower pursuit movements are difficult to learn if there is nothing to look at. Objects with good contrast need to be close enough and the luminance level at the optimal level to facilitate visual search and fixation. Sometimes it is helpful to dim the lights in the room and shine a focal light on the toy within reach of the infant (see Stimulation: Usual playthings)
Such a simple thing as a balloon functions well in early stimulation. It is a perfect learning situation if the ball is tied to the hand or foot of the infant so it moves when the hand or foot moves. Thus the infant experiences the sequence 'I did something and something happened, I did the same thing and again it resulted in the same thing happening'.
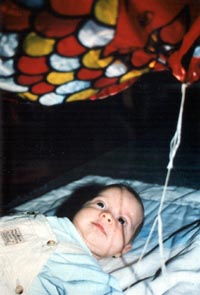

A large balloon of glistening metal paper is tied to the wrist of the baby. When the hands move the balloon moves and the child stimulates himself and learns about cause and effect early on.
When an infant is able to perform saccades testing of grating acuity with LEA GRATINGS or the Teller Acuity Cards and contrast sensitivity with Hiding Heidi is possible. The low contrast Heidi pictures demonstrate the parents and the care takers which contrast levels the infant responds to and at which distance. Observation of this test situation usually motivates everyone to communicate close enough and to increase contrast on the face with make-up (also men can use brown contour pen).
Grating acuity and contrast sensitivity measurements are useful tools for follow-up of visual functioning. The results of the grating acuity tests are given as cycles per degree and explained to the parents by showing the grating that the infant could resolve and at which distance that occurred. The result should never be given as optotype acuity because in visually impaired individuals there is no regular correlation between grating acuity and optotype acuity. I have a patient who has grating acuity 6cpd and normal contrast sensitivity at low spatial frequencies with grating tests but no measurable visual acuity with optotype tests due to infarction of both primary visual cortical areas soon after birth. In monkeys, grating acuity 6cpd can be measured after removal of visual cortex.
The use of grating acuity values for classification of vision impairment has no foundation in visual physiology and leads to great injustice if infants and children with grating acuity 3cpd are diagnosed as 'not legally blind', which means that they will not receive early intervention services. 'Legal blindness' has nothing to do with infants; their needs cannot be compared with those of working men.
Visual field is difficult to assess during the first few months because the infants attention is strongly directed to the centre of the visual field. Small illuminated toys in a dimly lit room may elicit a response better than the traditional white Sheridan balls.
This infant is much delayed in her early development due to hydrocephalus and hemiplegia. She is aware of visual information only in the middle of the visual field. See the video.
See the video.

The Sheridan rolling balls and balls on wand are still used in the assessment of detection acuity and visual field. The toys, chair, car and aeroplain do not function well because of colour differences. In Nordic countries the Moomintroll figures are useful test material and a collection of sweets (on the right) from all Nordic countries has good stepwise increase in size for testing detection acuity.
If no responses can be elicited to visual stimulation during the first few therapy sessions, it should be stressed that development of vision may be delayed. If an infant is called blind there is very little motivation to continue play situations that stimulate visual pathways.