Vision Care 3 years to 10th grade
[ 1-27 ]|[ 28-50 ]|[ 51-75 ]|[ 76-100 ]|[ 101-128 ]
Slide 1.

Vision care of school children has changed during the last fifteen years when children with different disabilities have become integrated in local schools. Instead of basic vision screening that has been the content of vision care given by the school nurses, we now participate also in the transdisciplinary assessment of vision for IEPs of children with special needs.
This lecture was given in Las Vegas, April 28. - 29.2004, as a part of discussion on development of vision services for school children. A discussion like this should be repeated after a few years so that all nurses are aware of the principles of screening, of individual assessment of vision and of referral practices. Deeper understanding of the content of the services and of the role of vision in the development and functioning of children leads to effective use of examination techniques and better quality of services. In several instances this improved quality of working saves time and money and therefore it interests also the administration of the services and insurance companies.
Although variations in vision screening are great, many central features are common in all countries. The discussions of these two lectures and in the short overview of vision services for infants and toddlers (0-3 years) get their special flavor from the traditions in Nevada and in Finland. In both places vision screening has defined its goal as follow-up of development of vision and early detection of deviations from normal development, much the same way as length, weight and hearing are measured exactly. Thus the vision services cover more than amblyopia screening. In Nevada there are also long traditions of participation of school nurses in assessment of vision of children with special needs. Because of these goals, measurement of visual acuity is done until threshold and nurses have experience in assessment of visually impaired children.
Since the discussions during these lectures were found interesting, they are made available to a larger group of workers in the field to further activate discussion and comparison of different vision services.
INTRODUCTION
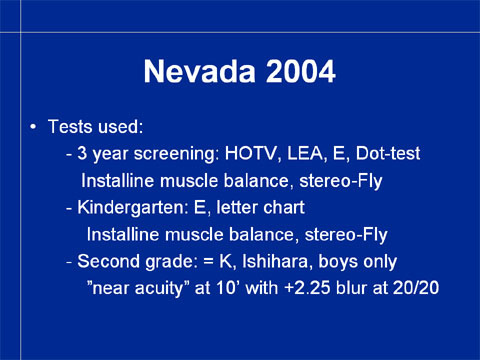
In Nevada, the techniques used in vision screening between 3 years and the second grade are now:
In the screening of the three year old children:
- visual acuity tests: HOTV, LEA, tumbling E and Dot-test
- Insta-Line muscle balance test
- Stereo-Fly, Stereo-Reindeer
In the screening of children in kindergarten:
- visual acuity tests: E and letter chart, Sloan letters
- Insta-Line muscle balance test
- Stereo-Fly, Stereo-Reindeer
In the screening at the second grade: the same tests as in kindergarten and color vision screening with Ishihara test, only boys.
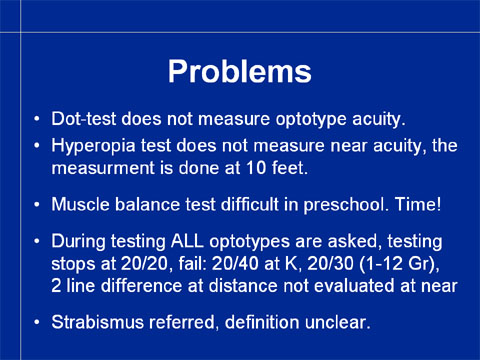
The use of several visual acuity tests often means that a child is tested with three different tests in the three test situations. Since each test measures vision slightly differently, the results are not comparable. Normally there is an increase in the visual acuity values by 1-2 lines between these measurements when the same test is used in each test situation.
The Dot-test (add manufacturer) is not a visual acuity test but an eye-hand-coordination test. The child is asked to point to the dot. Thus the visual task is to localize where there is a dot on the white surface, a parietal lobe function, whereas visual acuity measured with optotypes is a recognition function of the inferotemporal lobe.
Hyperopia test was introduced when the services were criticized for lack of near vision testing. Hyperopia test does not assess quality of near vision but may reveal higher than usual hyperopia. If hyperopia does not cause decrease in visual acuity and/or esophoria it does not need to be corrected and therefore hyperopia test is not particularly useful. This has also been the experience of the nurses. Since the test situation is experienced difficult and time consuming, its use could be discontinued. The same applies to the muscle balance test. Instead near vision line and single LEA Symbol tests are introduced. They can be used in assessment of all age groups because LEA SYMBOLS® (and LEA NUMBERS®) are calibrated with Landolt C. The other pediatric visual acuity tests are not calibrated with Landolt C. (The comparative studies with the ETDRS test are not calibration studies, ETDRS itself does not fulfill the standard of visual acuity test because the letters differ in their recognizability. However, ETDRS is the best visual acuity test with letter optotypes.) The LEA SYMBOLS® are used in the examination of adults with communication problems using matching, which is a true test of vision undisturbed by language or speech. The LEA SYMBOLS® can be used internationally and are, for example, used by the US Military Services abroad and in the examinations during the Special Olympics to avoid communication problems.
During the measurement of visual acuity, all optotypes on each line are asked in Nevada. This requires more time than if only the first/last optotype on each line would be asked. (Read the Instruction of the LEA SYMBOLS® VA tests.)
The pass/fail criteria could be re-evaluated.Only the picture of the Stereo-Fly or the Stereo-Reindeer is used in screening. Since there are in these tests also stereo images that require better stereo resolution and thus depict the level of binocularity better, and since many children can respond to these pictures, they should be used in the examination. Stereo tests are expensive and therefore they have not been accepted in many countries as a part of amblyopia screening. Since all nurses in Nevada have a stereo test, either Titmus Stereo-Fly or the Bernell Stereo-Reindeer, their use is recommended.
The guidelines of referral in case a child has strabismus should be defined. Since strabismus may lead to development of amblyopia, it needs to be included in the list of techniques to detect amblyogenic factors.
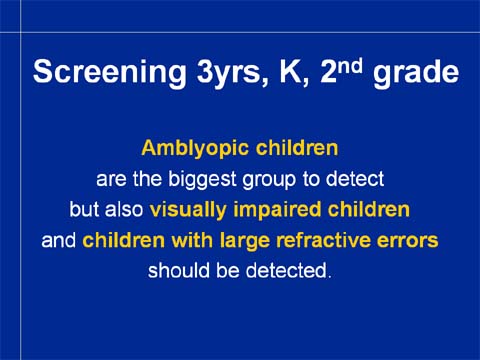
In the care of children of preschool age and still on the second grade level, amblyopia is the most important deviation from normal development to be detected. Visual acuity tests that are used in screening of amblyopia detect also a small number of children with decrease of visual acuity in both eyes, i.e. visually impaired children or children with large refractive errors. Among normally developing children visual impairment and large refractive errors are rare. Most cases of visual impairment are congenital and 60-70% of visually impaired infants and children have other impairments and disorders, so they should have been diagnosed before the screening at the age of three years.
Vision screening, like all screenings, concerns only symptom free healthy children.
If a child has intellectual disability, behavioral problems, motor problems, hearing impairment or any syndrome or disorder, the child is assessed with tests that are specific to that particular group of children. Most of these conditions are diagnosed during the first year of life and thus also assessment of vision by a paediatric ophthalmologist and by an early intervention team are performed as a part of the initial investigations. There should be information available from these earlier clinical investigations of each impaired child.
Healthy children should have information on their early development: check on red reflex and structure of the eyes at birth, eye contact at the age of 6-8 weeks, normal milestones in interaction, reaching for and grasping, recognition of family members and peers and no or minor alignment problems of the eyes. If they are not recorded earlier, it is wise to ask for this information when the child is seen for the first time at the age of three years or later.
In discussion of vision screening, we cover tests used at different ages, which functions are measured and observed, and who is referred to further assessment.
VISUAL ACUITY TESTS
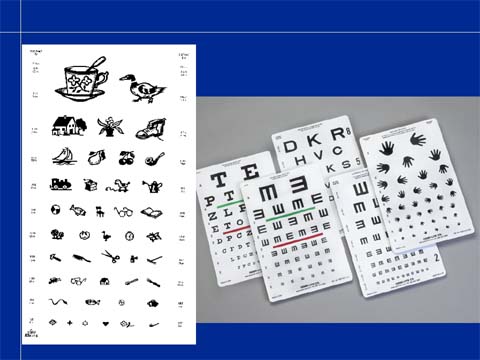
In the mid-70s, paediatric visual acuity tests were poorly calibrated and contained optotypes that required many other functions but recognition of the optotypes. It was therefore I started to develop visual acuity tests that would function better in both screening and assessment in 1976. The designing of the tests followed the advice given by the Department of Psychology at the Helsinki University: in order to have a sharp threshold of the measurement, the tests should be based on optotypes that blur equally and their size should be calibrated with the international reference optotype, which at that time was Snellen E. When the Landolt C became the reference optotype the symbols were calibrated once more, which was real hair splitting (see Calibration of LEA SYMBOLS® 1993).
The four optotypes that I designed were the first four pediatric optotypes that blur equally. This is apparent if you look at the tests at a distance where the lowest lines are blurred. You see the optotypes clearly until a certain line; below it all symbols are blurred to circles. The threshold is very sharp (not as in some letter and number charts where certain letters or numbers are clearly seen two lines below the line where other optotypes are blurred).
It was thought in 1970s that a distance visual acuity chart for 3-4 year old children, another for 5 year old and older, a near vision test with a standard line test and a more crowded test and single symbols tests for distance and near would be all that would be needed for good vision services. Later I have designed several other tests to meet the needs of different clinical test situations for children with special needs.
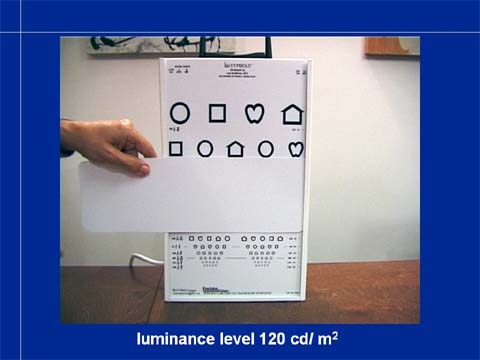
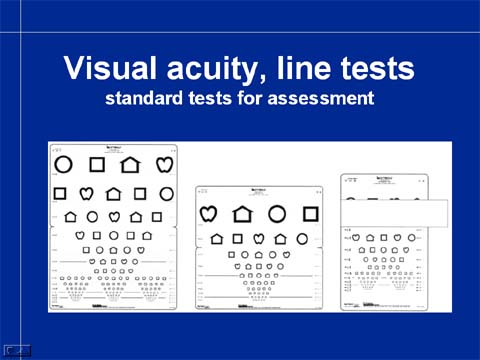
Translucent tests with back illumination have become standard in many states and countries because the luminance level is always the same and the lightboxes are easy to move from one screening location to the next. In Nevada the Insta-Line is the standard test and thus development of screening is based on it. Its test layout will be redesigned to allow use of five symbols on each line and the size of the symbols will be until 20/10 so that there will be at least one line that the child does not see. This allows measurement until threshold and thus makes it possible to detect a difference of two lines between the eyes.
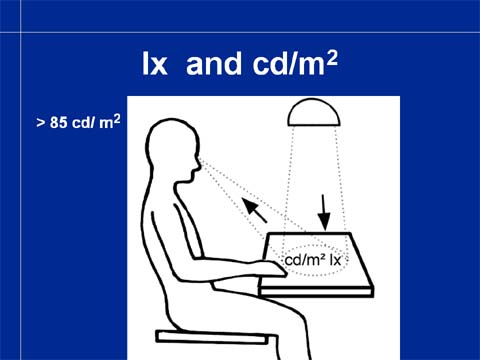
Visual acuity values become higher when luminance level increases until approximately 85 cd/m2. At higher luminance levels the visual acuity values first remain the same as at 85 cd/m2 and then at very high luminance levels dazzling decreases visual acuity.
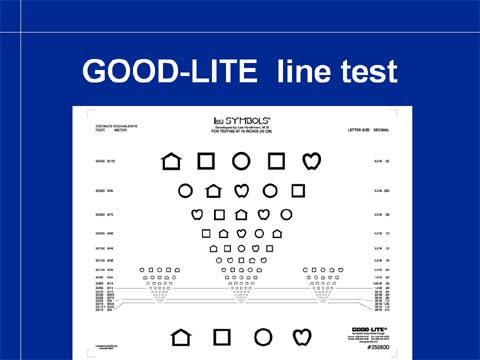
The near vision test is a miniature copy of the distance visual acuity chart.
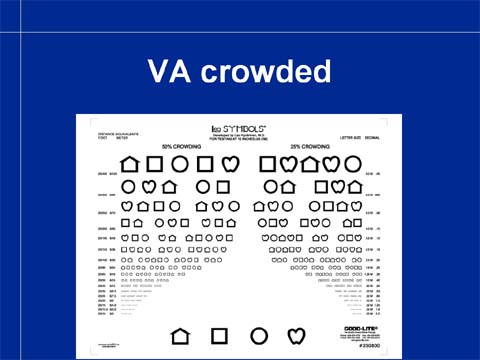
On the reversal side of the near vision card there are tests with less space between the optotypes. These tests measure crowding phenomenon more sensitively than the classical near vision test on the front of the test. Increased crowding is typical to amblyopia and several types of impaired vision and means that a child cannot keep optotypes and other details apart but they glide partially on top of each other. “They hug each other”, as a little patient of mine once described the phenomenon.
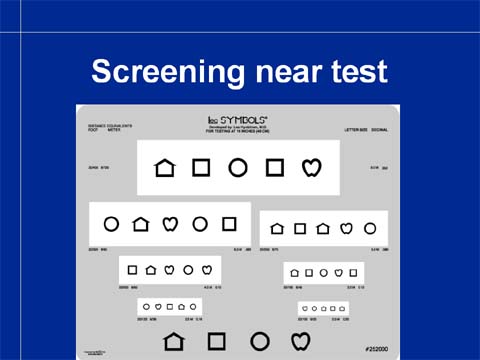
The standard near vision test is somewhat slow in screening. Therefore there is this screening version of the line test with more space between the lines. The test is easier for the child and the tester because it is easier to know, which line needs to be read. The visual acuity values are equal to those measured with the standard line test.
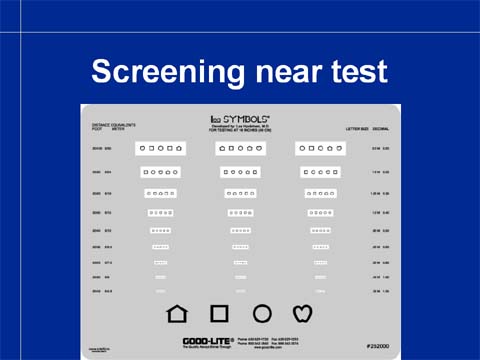
The smaller optotypes are in three well-separated lines so measurement until the threshold level is quick. The grey background dazzles less than the white background in assessment of children with visual impairment.
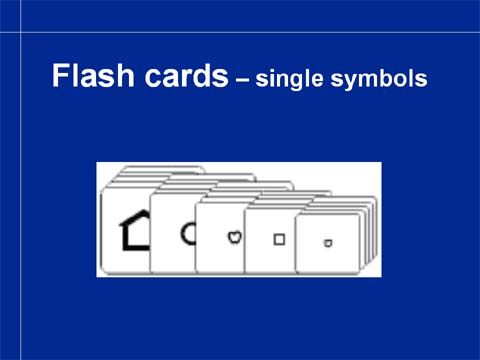
Children who cannot perform in the line test situation are tested using single symbol tests where there is one single symbol on a large white surface. Such single optotype is much easier to recognize even if fixation and accommodation are not normal. Therefore visual acuity values of amblyopic eyes measured with single symbols can be 2-3 lines better than those measured with line tests of the same optotypes. Even one line difference in single symbol tests might mean beginning amblyopia.
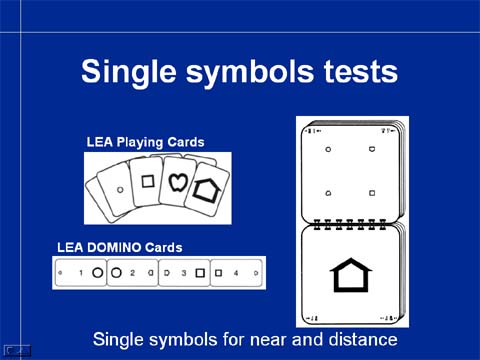
Single symbol tests are also in form of a small book for distance and as playing cards for near. The smallest symbols are in the LEA Domino Game that was designed for training of amblyopic eyes.
In this picture you see the three year-old girl playing domino game with the LEA Domino cards. There is patch on the right lens of the glasses to make the child to use the amblyopic left eye. A younger sibling observes the play situation and learns the symbols quite early. This is important because he might be in danger of developing an amblyopic eye and therefore follow-up of the development of visual functions should include measurement of visual acuity as early as possible.

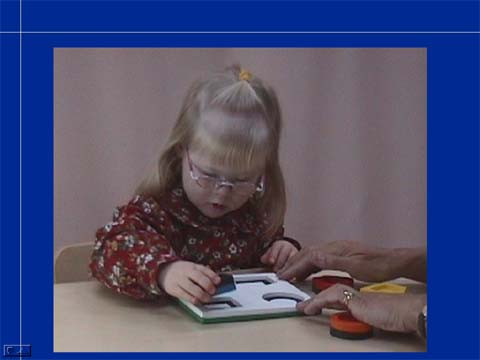
For training of the test situation I have designed the LEA Puzzle that is useful in training young children and children with special needs. At the same time it is a neuropsychologic test. We all learned match colors before we could match forms. Therefore there is the colorful side of the puzzle where the child can place the puzzle pieces by matching the colors. At the same time the child is playing with the forms (in color) and learn the locations of the different colors and forms on the puzzle board. With this training children can be tested with single symbols test at near when they are 18 months old. If also covering of one eye at a time is trained, as a part of the play, screening of visual acuity is easy and quick.

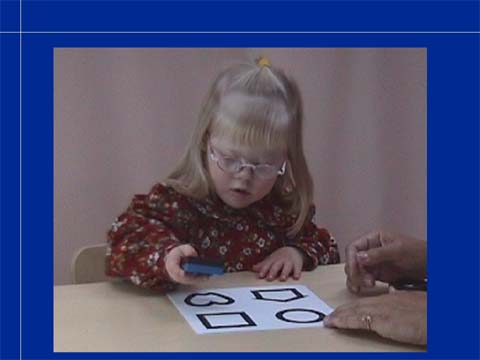
Like this little girl with Down syndrome, many children with special needs require a shorter or longer time to train for measurement of visual acuity with optotypes. Some children need to train with the puzzle board at the first grade. Since this activity is typical to toddlers and young children it can be included in their play situations in the day care and at home.
Slide 19.
Slide 20.
Slide 21.

Slide 22.

When the child masters the colorful side of the puzzle, the black-and-white side is introduced. When the child can play with the black-and-white forms, a much more difficult step in development is trained: comparing a concrete object with its picture, first the same size, then smaller and smaller. At this stage we are
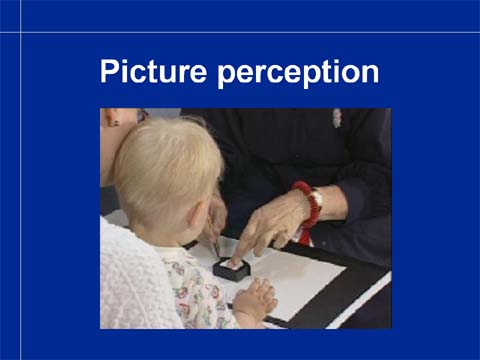
If the development of the concept of pictures representing objects is difficult, drawing around the child’s hand, foot, favorite toys, small kitchen utensils etc. is helpful. After that drawing around the puzzle pieces may make the comprehension of these slightly more abstract pictures possible.

Playing cards can be used as a part of occupational therapy and function as a fun test of single symbol acuity. By measuring the distance that the child uses to look at the symbols (preferably with your hand instead of a ruler) and knowing the M-size of the smallest symbols correctly recognized, the visual acuity can be calculated by dividing the distance in meters by the M-size. For more information, Instructions Section.
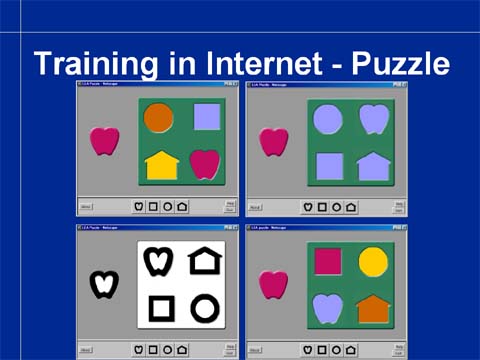
Children can play with the symbols also on the Internet on my homepage in Section "Games". This is a neuropsychological test where one can observe the child’s ability to match colors, forms in color and black-and-white forms.
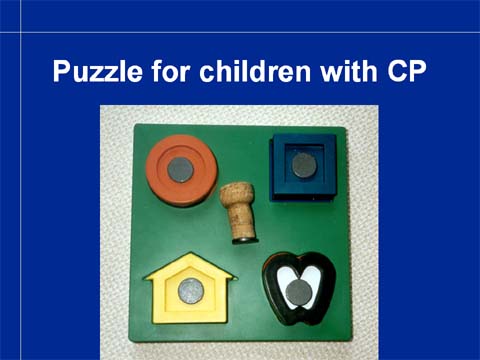
When we test children with CP, the LEA 3-D Puzzle needs to be modified by using small magnets on the puzzle pieces and on a champagne bottle cork to allow the child to move the puzzle pieces.
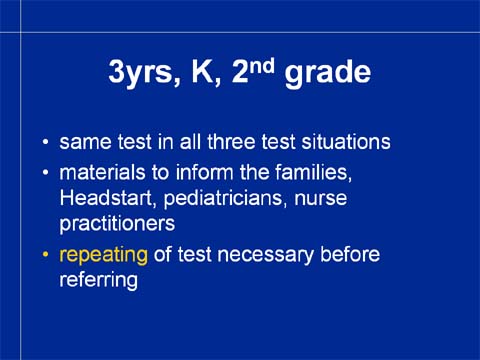
When the LEA SYMBOLS® tests are used, the same tests can be used in vision screening of healthy children during screening at 3 years, kindergarten age and at the second grade. Then it is possible to notice changes in visual acuity values. Normally, visual acuity increases by 1-2 lines between each measurement.
If the families and day care receive information materials on the importance of early vision screening and the children train the test situation, measurement of visual acuity becomes a quick and accurate procedure.
There is variation in the functioning of children in their performance during vision screening. Although a great majority of children has exactly the same results in repeated measurements, still at the age of seven years some children show a variation of plus/minus two whole lines in their visual acuity when the measurements have been made in the same room and with the same instruments. Therefore visual acuity values should e measured twice before making the decision to refer. (I have learned that it is the rule also in Nevada.)