Vision Care 3 years to 10th grade
[ 1-27 ]|[ 28-50 ]|[ 51-75 ]|[ 76-100 ]|[ 101-128 ]
OCULOMOTOR FUNCTIONS & STRABISMUS
In the vision screening before the school age and at the second grade we look for signs that could mean deviations from normal in the vision development.
Fixation and following/tracking are quick test situations that may reveal difference in the use of the two eyes. We look for unsteady fixation or fixation nystagmus during monocular fixation, irregular following movements instead of smooth pursuit movements.
Strabismus often causes amblyopia in the strabismic eye, especially in inward squint. Therefore testing for alignment with cover test is a valuable test.
We measure visual acuities with line tests because it is an effective way to detect amblyopia. Normal visual acuity does not exclude cerebral visual impairment, brain damage related impairment. Therefore a list of the most common symptoms of CVI could be used as a part of vision screening to diagnose also CVI earlier than it is diagnosed presently.
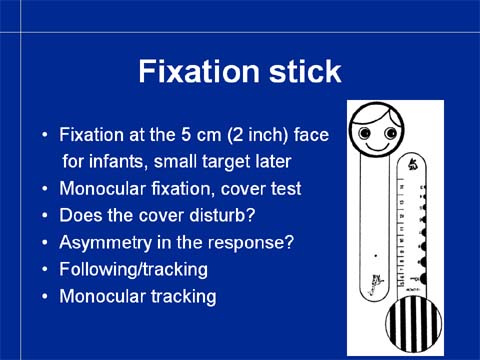
For the testing of fixation we need an accommodative target. I have designed my fixation stick based on the studies of Robert Fanz, who showed that picture of face with a diameter of 5 cm/2 inches interests a normally sighted baby at the age of three months and later so that fixation and following movements can be observed. The two smaller pictures, giraffe and bunny, are used in the examination of children at the age of 3 years and older because they are interested in
Slide 30.
Slide 31.
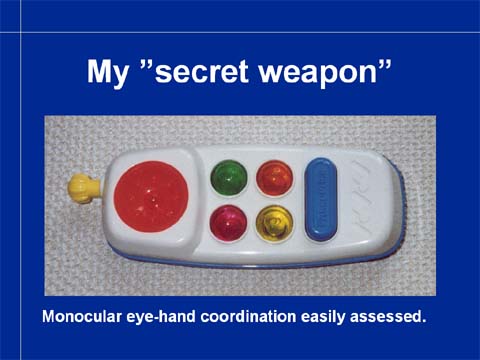
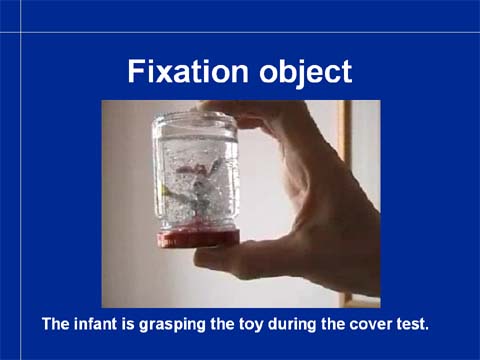
If the fixation stick does not interest a child, we use different toys to catch the child’s attention for long enough a moment so that cover test can be performed. My best toys are a baby food jar with a plastic figure glued on the lid and with “snow” flakes in water. Another good toy is a toy mobile phone in the assessment of infants. When the child is playing with any of these toys, he usually does not

In screening we usually use only direct cover test because alternating cover has been experienced confusing. With the direct cover test we can observe both tropias and phorias.
Video 1
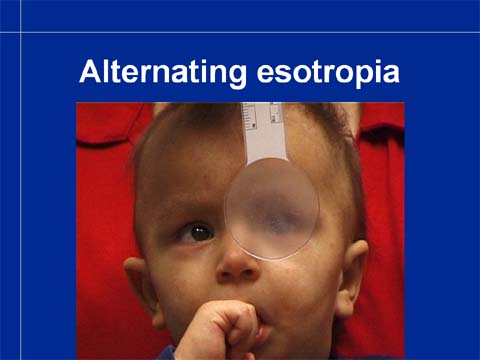
A few examples of cover test findings might make the test situation easier to understand. This first variant of inward squint, esotropia is the most benign type. The child can fixate with both eyes equally well, switches from one eye to the other eye spontaneously, so there is no greater risk of development of amblyopia. However, also this child needs to be referred so that the refractive status and central vision of both eyes are assessed more carefully. At the end of the sequence the infant’s gaze happens to fall on his father’s face and therefore remains in an inward position. His father namely responded to the eye contact by saying something and was more interesting a target than my fixation target. During the cover test we must allow the eye regain fixation before covering it again.

Video 2
This child has constant esotropia of the right eye. The eye is turned inward but fixates centrally when the leading left eye is covered. Fixation is stable. This eye may be amblyopic but the child uses the eye still quite well.

Video 3
You need to concentrate on watching carefully when the right eye is covered for the first time. Fixation with the left eye is unsteady, searching. Also during the repeated cover fixation is unsteady so it is likely that this eye is amblyopic, which it was found to be. However, it has recovered well during therapy.

In this case the camera angle has been chosen to be oblique so that the movement of the eye behind the cover can be seen well. During assessment the movement is quite well noticeable behind the cover but the camera loses much of the clarity of the image. Behind the cover the leading, dominant eye turns in and immediately takes fixation when the cover is removed.

If exotropia, outward squint lasts only a short period, a few minutes when the child is tired or is sunken in his thoughts, it does affect the development of binocularity in children who have their eyes aligned most of the time and have already developed strong binocularity with good stereovision. (Intermittent exotropia is a common finding in the listeners toward the end of lectures.)
Slide 44.
Slide 45.

Slide 46.
Slide 47.
Slide 48.
It is worth watching these slides over and over again. In order to make the training effective, the slides are here without the headings and in the PowerPoint presentation you have both variants. (The animations will be on the PowerPoint and on this text on the CD.)
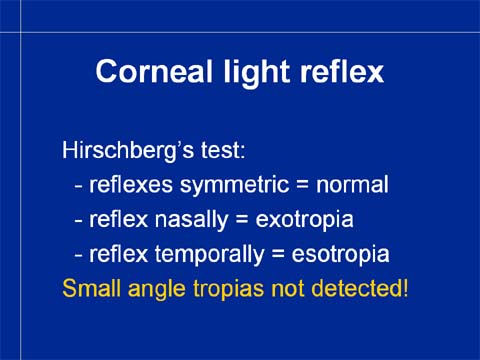
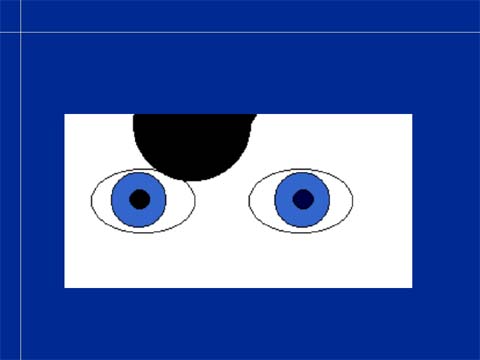
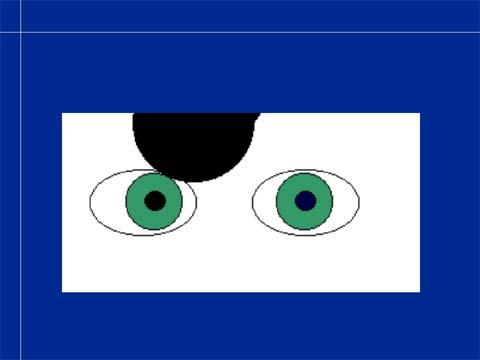
Hirschberg’s test or corneal light reflex test is a much-used quick test to detect exo- and esotropias. It does not reveal small angle tropias. If reflexes are symmetric and central the eyes are aligned or the angle of strabismus is small. If the corneal reflex is nasally, the child has exotropia. If the reflex is temporally, the child has esotropia.
VISUAL ACUITY BASED SCREENING

Visual acuity based screening has been the backbone of vision screening in the State of Nevada and many other states and countries for more than thirty years. It has nearly uniform structure in most programs. It can be started at the age of three years but at that age too many children react negatively to the covering of an eye, whereas at four years of age, nearly all children accept covering of the eyes in turn. The success of testing can be greatly improved if the three-year-old children have played covering-the-eye-games and played with the 3-D LEA Puzzle and the Playing cards. During these games the teachers and parents may have noticed that a child allows covering of one eye but not the other. This should be known as one of the signs of too big a difference in the function of the two eyes and thus a diadnostic sign for referral.
WHAT ARE WE TRYING TO FIND WITH THE VISUAL ACUITY SCREENING?
Since we have already detected children who have tropias
either with the Hirschberg’s test or the cover test, the children to
be found with the measurement of visual acuity are
- Children who have so small angle strabismus that it
has not been noticed in the previous two tests, but which has lead to
asymmetric development of visual acuity or
- Children whose eyes are aligned but have unequal
refractive errors and therefore also unequal visual acuity; Anisometropia may have caused amblyopia in the eye with more blurred image but this is not very common at the age of four years. If the child has symmetric corrected visual acuity and normal stereo acuity, the family may decide not to buy glasses but check visual acuity at the kindergarten after a few months hoping for emmetropisation of the eye with higher refractive power.
- Children with decreased visual acuity in both eyes either because of large refractive errors or visual impairment of both eyes due to disorders in the eyes, in the visual pathways or in the higher visual functions. This is the smallest group because nearly all visually impaired infants and children are nowadays diagnosed early among the children with other impairments (60–70% of visually impaired children have at least one other impairment or disorder or chronic illness). We need to be aware of the group of children with hereditary retinal disorders who may have been symptom free until 3–5 years of age. Most of them have symptoms of beginning difficulties in dim light so this should make the persons taking care of the child to start questioning. Also, there is the small group of children with storage diseases who may have had perfectly normal development until 2.–5. year of life and then lose some of their visual acuity and often at the same time develop behavioral problems. Therefore children who “do not concentrate” or “do not co-operate” should have their sensory functions carefully examined before they start receiving any therapies. This, not because the therapies wouldn’t be helpful, BUT because the child’s condition needs to be diagnosed.
It is generally accepted that the difference between the visual acuity values at distance needs to be at least two lines to warrant referral. The referrals can be further restricted to cases where there is the same difference also in the visual acuity values at near. Since myopia is rather rare in the preschool population, this addition to the measurement battery does not notably affect the screening before school age, whereas it markedly reduces the number of wrong referrals in the teen-age population. Therefore it should interest the administration of the services.
When I started as the ophthalmologist in charge of the schools in Helsinki in 1983, the pass/fail limit was visual acuity 20/30 in one or both eyes. Therefore more than half of referred children had so mild myopia that it did not require correction. Several parents were angry asking why they had been asked to take half a day off from work (unpaid) to come with the child to my office when nothing needed to be done. I felt that it was an important question and introduced the use of near test to find out that a child who earlier had had visual acuity 20/16 in both eyes and now had 20/16 and 20/30 at distance and 20/20 in both eyes at near, that (s)he did not have anything else but beginning myopia. Namely, if the child has 20/20 visual acuity at near in both eyes, then only myopia can be the cause of decreased uncorrected distance visual acuity. This decreased the number of referrals in Helsinki to one half of what it had been and we got time to assess all special needs children at their schools together with the school nurse and the assistants whom the children wanted to be with them during the assessment.
It is important that health care services do not refer children who do not need to get glasses because there is a risk that a child may get very weak glasses that remain mostly in a drawer. This happens in all countries, especially if the doctor has any economic interest in selling the glasses.
In the control of the quality of referral services, it is important to get reports from the doctors. Also, if children are asked to have follow-up by the eye doctor for no good reason (it has happened that nearly all children were asked for follow-up in six months) the situation needs to be discussed with the local eye doctors and the administration.