Vision Care 3 years to 10th grade
[ 1-27 ]|[ 28-50 ]|[ 51-75 ]|[ 76-100 ]|[ 101-128 ]
VA SCREENING TECHNIQUE
The child needs to be able to match or name the symbols. Matching requires the concepts similar/different, which can be trained. When naming is used ANY NAME is OK. Children must not be corrected, even if the name might be as strange as “bunny ears” for apple. The name may also change. The house is in the larger sizes house and then becomes a “dog house”; similarly apple may become berry in the smaller sizes.
The order of measurement that I have found
to
function well, is following:
- Binocular near visual acuity, the most important VA for
learning
- Binocular distance visual acuity, the functionally
important VA value at distance
- Both monocular visual acuity values at distance, usually the RE first, then LE, except when the child reacts clearly negatively to covering of the left eye (which may be the non-amblyopic eye).
- If there is difference between the monocular values at distance then also monocular values at near are measured.
Children perform best in vision screening if it is fast and easy. Therefore it is important to make it child-friendly:
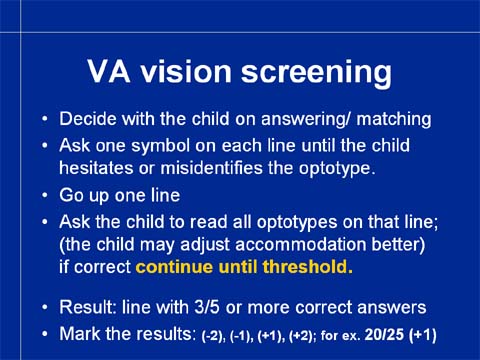
Ask the child first, whether he wants to use 1) the translucent key card (or the easier LEA Puzzle board tactily) to point at the picture on the key card he sees on the test, or 2) use the names of the symbols. If the child chooses the names, point on the symbols on the uppermost line and decide with the child, which names the child wants to use. Respond with a low key “Those are nice names” even if the names might be funny (the “apple” has had more names than the other three symbols, “heart”, “bunny ears”, “slippers”, “butterfly”, “butt”, “rump” [do not allow the mother to interfere]; the most unusual name for “house” has been “mouse”, “don’t you know? on the screen” ).
Ask the child what is the first symbol on each or each other line. When approaching the threshold ask also “And what is next to … (the name that the child used for the first symbol). This prepares the child to read along the line. Do NOT point, it makes fixation easier. Rather cover the line above the line to be read if the child has difficulty in fixation.
When the child makes an error or hesitates, move up one line and ask the child to read the whole line. Support a young child by saying “And next to the…” after each symbol. If the child has answered incorrectly, say “And after that there is?” This helps the child to concentrate on looking on the line and thus keeps the eyes correctly focused. If the child looks at you, focusing is likely to change. Therefore, if the child does not see the symbols on the line where two or three symbols were already seen, go back one line and ask the child to name the first symbol and then go back to the line below. Visual acuity is the value of the smallest line, on which at least three out of five symbols are read correctly.
When writing down the result, the most exact way is to write the number of symbols that were read correctly; i.e. if 20/25 line was read correctly and one symbol on the 20/20 line, the result is 20/25(+1).
In Finland, we use the same rule as in Nevada: if a child does not get a normal result, then the measurement is repeated either by the same person or by another person, whom the child knows well, usually the school nurse of his/her own school. It is important to know that visual acuity values of normal well-functioning children may vary two lines worse or better than the value measured in the same room with the same instruments a week or two before. The number of these children is not great but they are there in all populations.
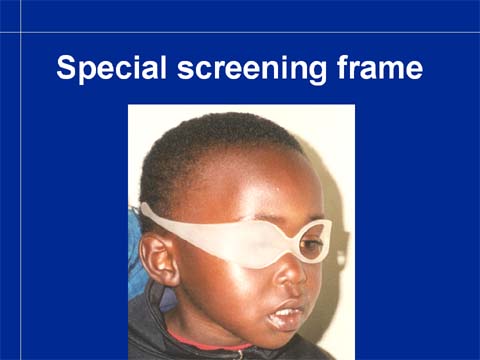
Covering the eye is often difficult. Therefore we have tried to develop different ways of covering. One of them is this special frame with straight sidebars, the other much-used technique is having two pairs of sunglasses with one lens removed in each and the other covered.
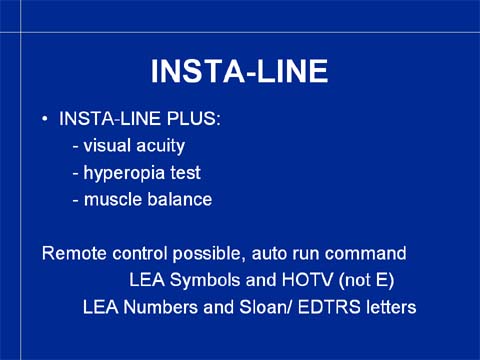
In the INSTA-LINE test visual acuity can now be measured until 20/20. It will be (and has been) changed so that the smallest symbols/numbers/letters correspond to 20/12,5 and there are 5 symbols on each line. The muscle balance test and the hyperopia test that have been criticized in this lecture will not be integral parts of the test system, but will be available.
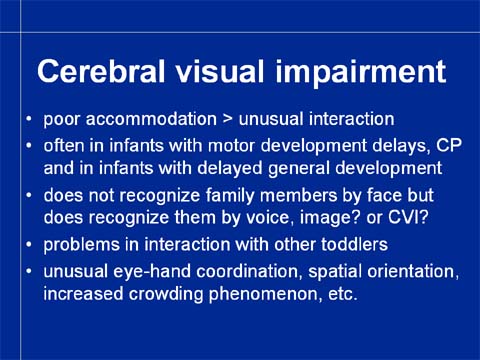
Vision screening should detect all different types of visual impairments. The rapidly increasing number of young children with cerebral visual impairment, CVI, needs to be diagnosed earlier than today. Too many of these children come to school without early intervention services and enter school system that is not prepared to take care of them.
Present visual acuity screening detects only a part of them, so we should add to our screening techniques a questionnaire on the most common symptoms of CVI. Also we should follow the recommendation that all infants with other impairments and disorders need to be assessed, not screened, preferably as a part of the initial investigations also for their sensory functions; most often during the first year of their life. This would be the most effective way of getting all visually impaired infants within the early intervention services. It requires further education of both pediatricians, pediatric neurologists, ophthalmologists and audiologists.

At this moment we wanted to have a break.
This is the question for the second part of this discussion.
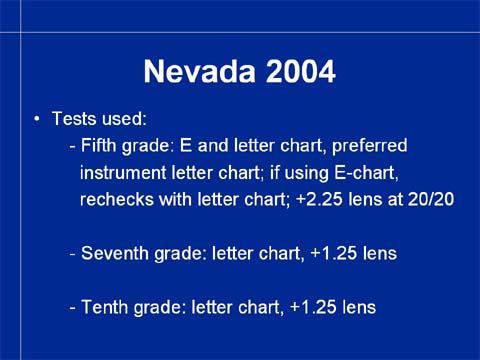
This is the present situation in Nevada. There are three mandated screening times during the period when the majority of children who are going to become myopic start to move on the myopic side.
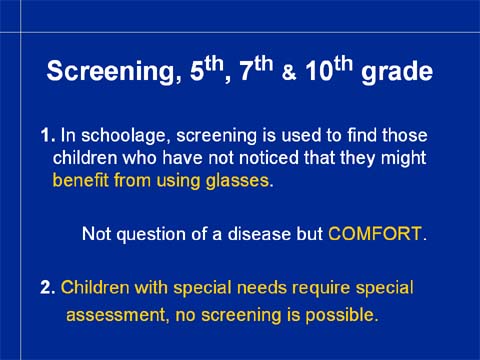
Screening in school age after the second grade is totally different from vision screening in preschool and still on the second grade. We are no more searching amblyopic children or any other treatable condition but children who have not themselves noticed that they could benefit from using glasses. As it is written in the slide: the question is not a disorder or disease but VISION COMFORT at school.
Since the question is of vision comfort, we need to define what is needed for comfortable seeing at school.
Children with special needs have such a great variation in their vision problems that no screening functions, Similarly as before the school age, these children need to be examined by their ophthalmologist/neurologist/audiologist and followed by their team at intervals that are decided individually for each child. Children with CVI are often the least understood students at all schools because people cannot understand and believe that a child may function normally in most visual tasks and yet be blind in other visual tasks.
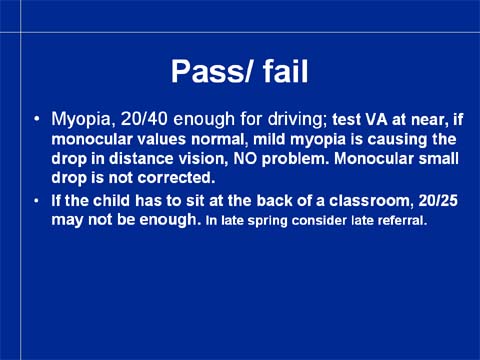
The technique used in measurement of visual acuity is the same as in preschool screening. Since the children should not be referred too early or too late, we need to define what is needed for good functioning at school. For adult person 20/40 visual acuity is accepted as good enough for driving, therefore one might think that it could be an acceptable pass/fail line at schools as well. However, if the student is allowed to sit in front, a visual acuity of 20/60 will be enough. On the other hand, if a student is sitting in the last row of a class of 40 students and the handwriting of the teacher is not good, even 20/25 will be too low. This means that we need to know the schools and use common sense more often than we are used to.
Now the near vision test becomes important. If there is a drop in the visual acuity value (compared with the previous screening) also in the second measurement, we measure the near vision acuity. If the near vision values are normal and close to the previous ones or better, the change in the distance vision is related to myopia. The child has good vision, is only a bit myopic. Myopia is not a disease that needs to be treated but may cause discomfort, so we need to know whether the child has discomfort in reading from the blackboard or whiteboard. If not, (s)he will not buy glasses or use them if they are bought but rather squeeze to see the smallest details. Squeezing is not dangerous and at their age they do not get wrinkles. Their myopia will not develop faster or more slowly if they don’t use glasses.
Summa summarum, there isn’t one clear pass/fail line but the comfort line.
Somebody asked: what if one eye is more myopic than the other? Say that the one eye has visual acuity of 20/25 (previous 20/12) and the other eye 20/100? This is no problem at all. Usually the more myopic eye is preferred in reading and the less myopic eye when looking at distance. Thus the student needs to accommodate very little when looking at near, sees well both at near and at distance – and will do so for years, in some cases through their whole life and will never need glasses. Again, comfort is the deciding line. As long as the child has no discomfort (s)he is not referred. If (s)he has discomfort (of any kind), either it is treated by the school doctor or the child is referred independent from what the visual acuity values are.
Somebody said that your rules ask you to refer all children who have VA values below a certain limit. This is something what I would like to see you reconsidering. If health care personnel refers students who do not need glasses to doctors who a likely to give them weak glasses that the student does not need, then the personnel does not function as proper health care personnel.
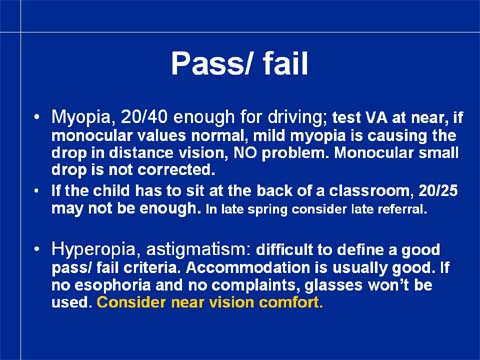
If it is impossible to define a VA value for pass/fail in case of myopia, it is even more difficult to define a VA line for referral in case of hyperopia or astigmatism. If the student is symptom free and has no esophoria, I would not like to see him/her in my office.
Question: But if the student has headaches? – A student with headaches shall not be screened but treated. The causes of headache are many; lack of glasses is not the most common but the breakfast. We have as a rule that a student must eat, sleep and be active outside according to the recommendations given by the school nurse for two weeks, and the possibility of poor ventilation of the sinuses, disturbances in the bite and the neck-shoulder problems have been examined and ruled out, before a referral to the consulting eye doctor can be considered. Now a day it is common that parents would rather have their child treated by a doctor than accept the trouble of bringing up the child to follow healthy habits.
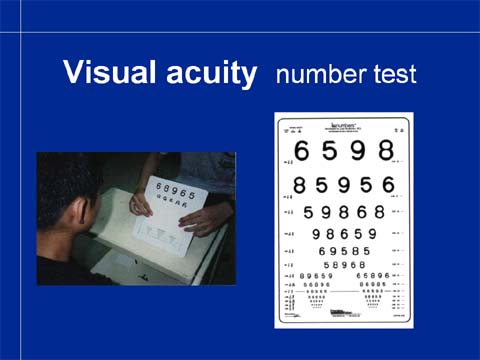
The tests used for screening are based on the LEA NUMBERS® or the EDTRS letters. Children older than seven years like numbers best. Letters add one more brain function, reading to the test situation. Numbers are also internationally acceptable, whereas the Roman letters are used in a limited area. (In Finland we are aware of this fact because east of our eastern border Cyrillic letters are used, farther east hundreds of different languages with their different characters are the reality. The LEA NUMBERS® were designed for international studies in occupational health.)
I would like to stress once more that the use of the near vision test helps us to find out that there is no other change but beginning myopia when there is a drop in the distance visual acuity value.
Someone brought up screening of children who have glasses. Of course we measure their vision but their care is not based on the screening pass/fail but when they feel it worthwhile to pay for another pair of glasses. To clarify this point I would like to tell a true story of a Finnish bright boy who got his second pair of minus lenses. He said to his mother:” Without my glasses I see that there is a tree on the yard. With my old glasses I see all the branches, even the thin branches. With the new glasses I see every single leaf. Do I need to see every single leaf?”
This brings us to the next slide and to the “What is important in the visual information?”
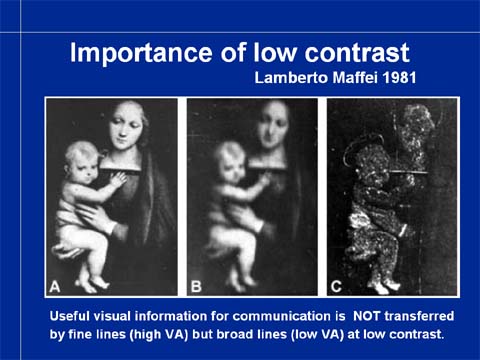
This slide depicts three photographs. The picture on the left is the original photograph. The picture in the middle was kindly made for my teaching by Lamberto Maffei in 1981. He filtered, removed the fine lines, so in this picture there are no lines that correspond to high visual acuity. The picture to the right contains only the fine lines. We all experience that there is more useful visual information in the picture in the middle than in the picture to the left. This is one of the most important slides of this lecture. If you remember that important information for visual functioning is NOT close to 20/20 but 20/200 and at low contrast, then you take more calmly the small changes in the high contrast visual acuity values that you measure.
Visual information at low contrast levels requires broad lines, large forms to be transferred through the visual system as we see in this picture. The fine lines carry only high contrast details. The low contrast information is the functionally important part of visual information in communication – the shadows on our faces are faint, communication is based on low contrast information in motion. Low contrast information is also important in orientation in space, especially when there is a demanding condition like fog or rain.
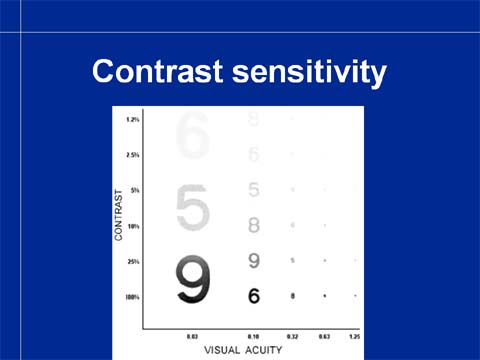
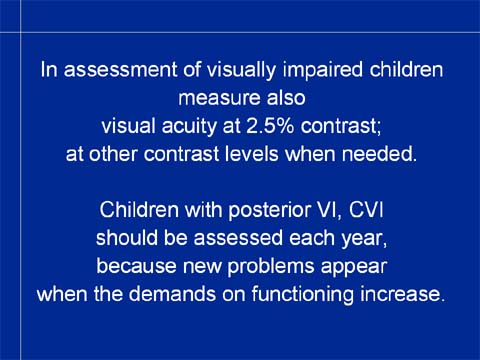
Whenever a child has any problems in seeing we should assess how the child sees at low contrasts. It is now easy because the low contrast visual acuity charts are equally easy to use as are the usual charts at high contrast. Measurement of visual acuity at low contrast, most often at 2.5%, takes less than a minute and costs very little.

With this short introduction into contrast sensitivity we are ready to start to discuss the other important part of vision care at schools: children with special needs.
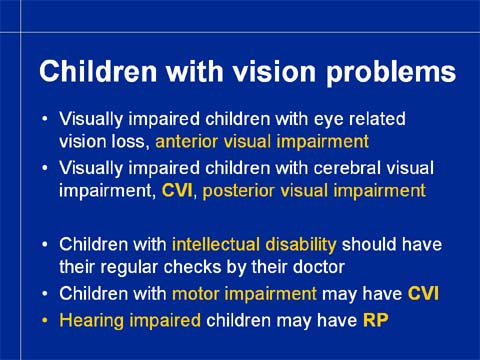
Among the visually impaired who are integrated in the local schools there are two different groups: 1. Children with only visual impairment and 2. Children with additional impairments and disorders.
Visually impaired children with anterior visual impairment and without other disorders have a well-established service system at local schools in many states, especially the totally blind students. However, children with useful vision are still categorized based on their visual acuity; and there are no rules how visual acuity should be measured. Quite often only distance vision has been measured with single symbols, letters or picture charts. The functionally more important near vision and visual acuity at low contrast levels and optimal text size have not been assessed. Even vision teachers may deny their services to children, whose visual acuity is better than 20/70 without assessing the child more carefully.
If a child has corrected visual acuity below the normal range, 20/32, then at least visual acuity at 2.5% contrast should be measured and the vision teacher should help the classroom teacher to test the optimal text size. It is possible that the measured visual acuity depicts such a small island of vision that it cannot be used for reading and thus functional visual acuity is much lower. All visual functions should be reported by the child’s ophthalmologist and retested at school.
Children with pure cortical visual impairment, loss of one or a few cognitive visual functions are the least well-understood children almost everywhere. If a child has face recognition or perception of facial expressions as the only loss (s)he is in danger of being diagnosed as autistic and children with recognition of geometric abstract forms or eye-hand coordination as their only problem are diagnosed as mentally retarded when they may not learn to copy even basic forms. It should be well known that it is not possible to be dumb in only one function. Uneven functional profile should always make us ask “Why cannot this child perform in this function while (s)he performs normally in many other functions?”.
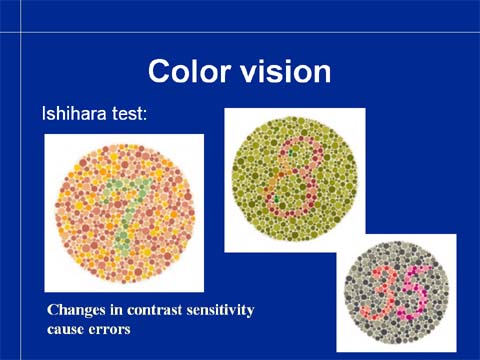
Colors are used in teaching materials and therefore we should know how students see colors. You are used to use screening tests like the Ishihara test in screening for hereditary benign color vision deficiencies. Screening tests are so sensitive that they pick also children with normal color vision. Therefore all abnormal screening test results should always be retested with quantitative color vision tests. (I take it for granted that you never use the term ‘color-blind’. If you do, this is the time to stop using this misleading term. Children with color deficiencies most often see colors quite well but confuse some colors.)

Quantitative color vision tests are sorting tests that show the confusions between colors.
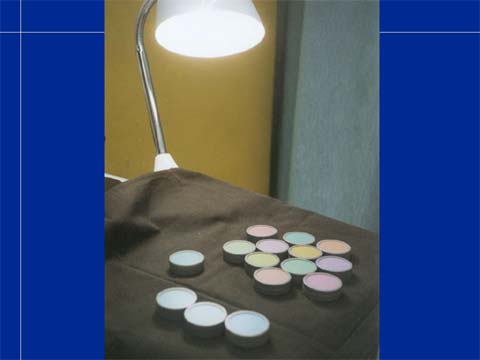
Like the screening tests, they are also performed at correct color temperature of higher than 6000K, in bluish grey light. This kind of light we have at a window facing North on a day with light overcast at noon (=international recommendation for illumination during color vision testing) or under special day light bulbs and rod lamps. Other light fixtures in the room are best switched off.
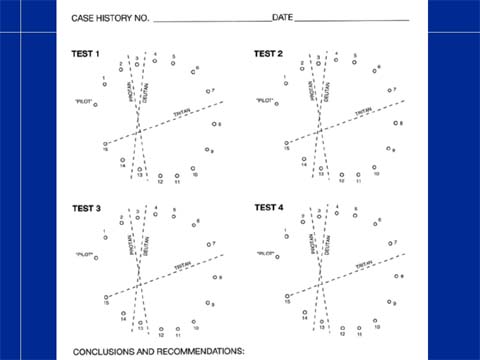
The results are recorded on special
recording
sheets based on the numbers on the bottom of the color caps. A line is
drawn from one number to the next as they are in the row of caps that
the child has chosen as the best fit so that the next color is the
closest in hue.
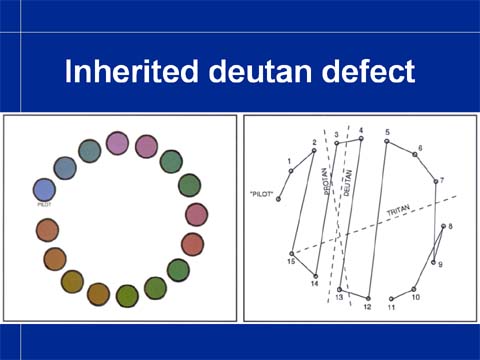
In case of a deutan defect the child has correctly chosen caps 1 and 2 but then felt that the purple cap #15 is closest the blue cap #2. After #15 he has chosen #14 and then #3, #4, #13, #12, #5 and after that the caps are in correct order except one small confusion. The big jumps from one end of the color circle to the other are regular and follow the deutan axis, so we call this kind of color deficiency deutan. It is the most common color vision deficiency.
Inherited color vision deficiencies may occur also in visually impaired children but they may have also acquired color vision changes due to disorders in the retina, optic nerve or in the cortical areas of color perception.
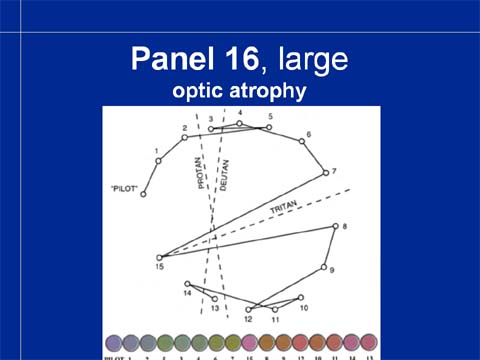
When color vision is abnormal due to optic atrophy the errors have another axis than in the inherited regular deficiencies. Now there is patchy loss of color information in the central visual field. The test result may look like this when the large LEA Panel 16 test caps have been used. The errors are in a blue-yellow or tritan axis.