Vision Care 3 years to 10th grade
[ 1-27 ]|[ 28-50 ]|[ 51-75 ]|[ 76-100 ]|[ 101-128 ]
Slide 76.
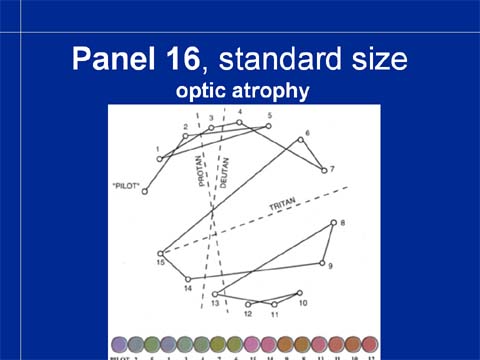
When the small color surfaces are used to measure color vision in the fixation area, there are more errors in the test result of the same boy with optic atrophy, again roughly in the tritan axis.

The fastest way of testing that at the same time prevents the child from touching the color surfaces is this: show the color cap next to the other caps and ask the child to point to the cap that is closest in color. The child must not touch the color surface. Since it is costly to refer children for quantitative testing by an optometrist or ophthalmologist, a quantitative color vision test would be a sensible investment.
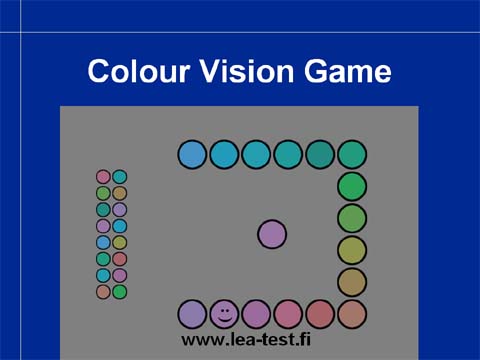
Children can train for color vision testing on the Internet where there is this color vision game on my homepage. It can be played also in the classroom so that the teachers see which colors are confused. Although this game is not a formal test, it is a good demonstration of color vision problems at school.
Colors that are easily confused should be separated from each other by a black or white line in teaching materials. Otherwise the colored area that we see as two different colors will be seen as one. If the color difference is critical in the task, then one of the color areas should be colored darker so that the child can use luminance contrast to see the difference between the color areas.
These three functions, visual acuity, contrast sensitivity, and color vision need to be assessed in all children with special needs. Visual field is more difficult to measure at school but observations on use of both peripheral and central visual field are important. They will be discussed in conjunction with brain damage related visual impairment and retinitis pigmentosa.
The foundation in our assessment of “functional vision” (in 2012 called visual functioning) is this document “Management of Low Vision in Children” that was written after the workshop arranged by WHO and ICEVH (now ICEVI) before the world conference in Bangkok in 1992. It is the first official document that stresses the need of assessing the effect of impairments on functioning, which is now the core message of the International Classification of Functioning, Disabilities and Health, ICF-CY (WHO 2007). The pediatric ICF is still on the drawing board. While the ICF for assessment of adult people does not recognize multi-impairment, not even deaf-blindness, we hope that the pediatric ICF will depict the life situation of children (60-70% of visually impaired children have at least one other impairment or chronic illness and multihandicap is common; its exact prevalence is not known).
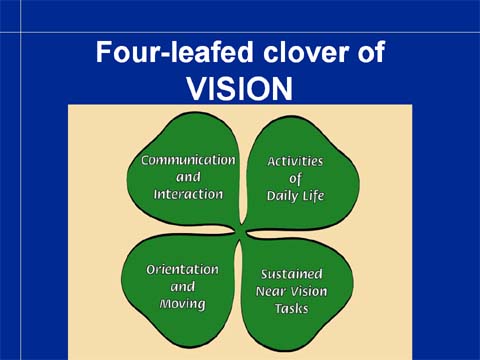
The Bangkok recommendation stresses the need of assessing the effect of visual impairment on all areas of functioning. The four main areas of functioning (that are not affected by local cultural differences) are 1. communication and interaction, 2. orientation in space and movement, 3. activities of daily life, and 4. sustained near vision tasks. I designed this four-leafed clover of visual functioning so that we have an easy to remember logo for functional assessments.
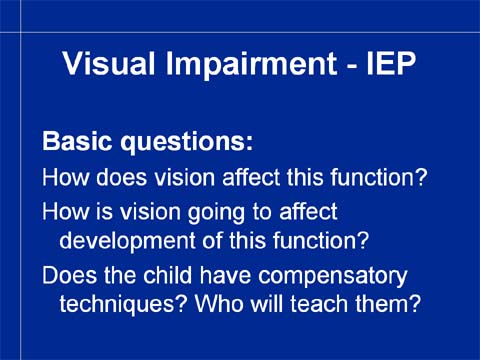
In each of the four main areas we answer these basic questions:
Does visual impairment affect this functional area, has it affected and does it affect now? If it does, in which ways?
Is visual impairment going to affect this child’s development in this functional area? If so, in which ways?
Does the child have compensatory techniques and strategies to cope with visual impairment? Which other strategies should be learned? Who is going to help the child to learn these strategies? Do we have a specialist among us or do we need to find one from centralized services?
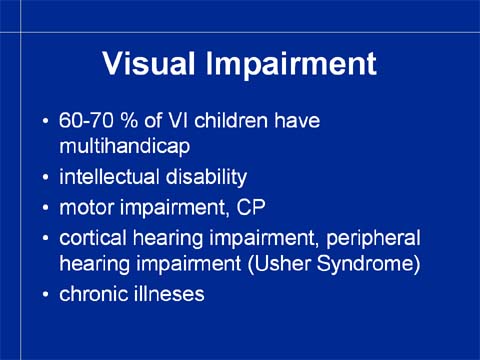
Since visually impaired children so often have other impairments and disorders we need to pay attention to these other impairments when planning our assessment. The three most common other impairments are the intellectual, hearing and motor impairments. The structure of visual impairment varies in these three groups of children so they are described as separate entities. When a child has three or four of these impairments then, of course, each of them affects the assessment techniques.

Visually impaired children with intellectual disabilities have more treatable eye conditions than normally developing children. For example, cataract may be present at birth, may develop before school age, in teenage or in young adults without any obvious external cause. Therefore assessment of vision is necessary every year until school age and then on the 1st or 2nd grade and on the 7th or 8th grade and whenever there are signs that may be related to problems in using vision.
Large refractive errors are more common in this cohort than other children, accommodation is often insufficient and emmetropisation is weak.
In many schools we see this group of children having clearly poorer quality of glasses than other children. This is a problem that we should pay attention to and send the child back to the optician with a letter saying that too big or poorly fitted glasses are not accepted in the care of children.
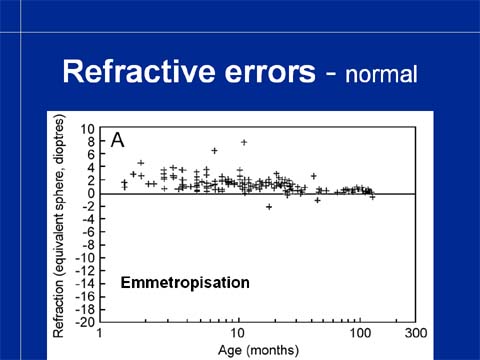
Emmetropisation means that refractive errors decrease when the eye grows so that at the time of coming to school refractive errors of most children are very small. How the eyes “know” to grow toward smaller refractive errors, is not known. Emmetropisation is a reason for not fully correcting refractive errors in preschool age if it is not necessary for treatment of strabismus or other conditions.
In this slide of Margaret Woodhouse et al. we see this phenomenon: refractive errors become smaller and smaller when children grow.
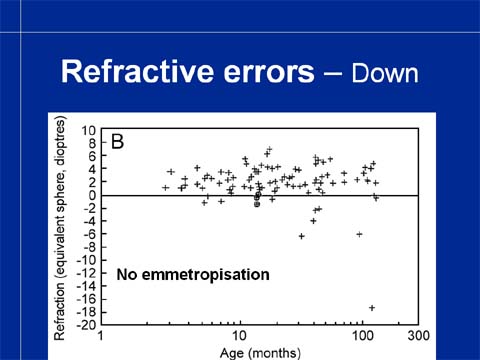
Emmetropisation does not occur in children with Down Syndrome (Margaret Woodhouse) and among them large refractive errors are more common than in other children. These children were examined only once for this study and their refractive errors have been present from infancy. (For example, the child with –18 myopia did not develop it at the age of 10 years, it was never measured before.)
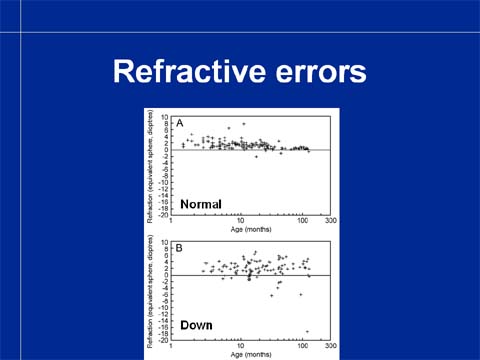
We see the difference between normally developing children and children with Down Syndrome when we place these two pictures next to each other.
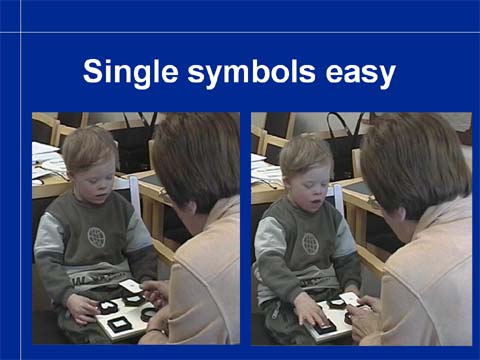
Testing of children with intellectual disabilities uses tests that correspond to their communication and developmental level. Still at the beginning of school age many children function well in testing with single symbols but...
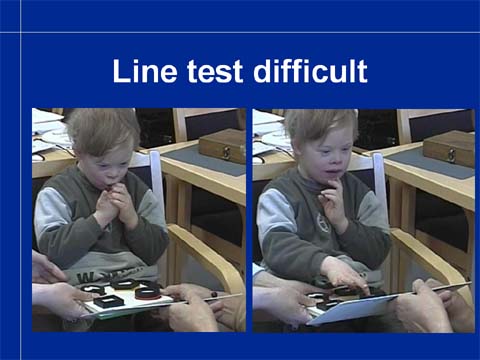
...have difficulties with line tests even when the pediatric LEA SYMBOLS® are used.

For testing at different distances and in different communication situation there are now several single symbol tests. The most often used is the Single Symbol Book. It requires that the child can either name or match the symbols. If the child has only yes no answers or can point with hand or foot or gaze, then the Flash Cards are used.
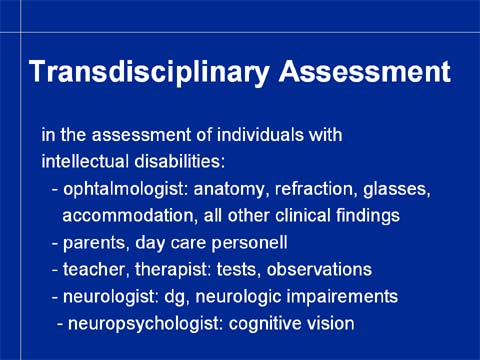
In the assessment of all visually impaired children we use the well-known basic plan of transdisciplinary assessment. It means that everyone in the extended team can and is willing to use the same basic tests so that information can be gathered from different functional situations and is also willing to share the information with the other team members.
The ophthalmologist is the source of basic information on anatomy of the disorder, refraction, glasses, accommodation and other ocular motor functions.
Parents, day care personnel, child’s assistant, therapists and teachers can repeat measurements of visual functions and make observations on the functions of the child. They spend more time with the child than anyone else so they are an important source of information.
In an ideal situation, the child’s pediatrician is the person who helps the family to collect and sort all the information from the many specialist consultations that these children have. The report of neurologist is often of special interest because visual impairment is so often also a neurological disorder, the use of visual information deviates from normal.
If there is a neuropsychologist available, it is often very helpful.
Video 4
This short video shows how well testing functions, when the tester is a special kindergarten teacher whom the child knows well. This child does not yet talk and thus supporting signs are used in the communication. Notice that the child signs “good” when she has been able to answer correctly. It is important that children experience success in test situation. Because the LEA SYMBOLS® all blur equally, the tester detects the threshold without the child experiencing a failure. (As I say “My children never fail.”)
Video 5
Educational assistants are important participants of the team. Assessment of this child without the assistant would be impossible. The tester is the itinerary vision teacher. First the puzzle pieces are compared with the large pictures on the key card so that it is confirmed that the child can match a three dimensional object with its picture. Then the teacher asks "what is the first symbol on each row". She covers the row above to make it easier to the child to know where to look at. This is the first time the child is assessed so he can concentrate to perform the task twice, which is a good result in a test situation. He will now train with the
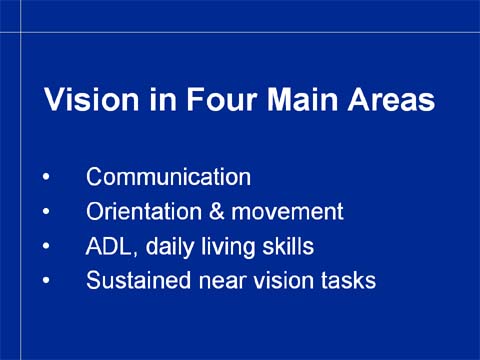
All test results and observations are used to assess the role of vision in the four main areas of functioning.
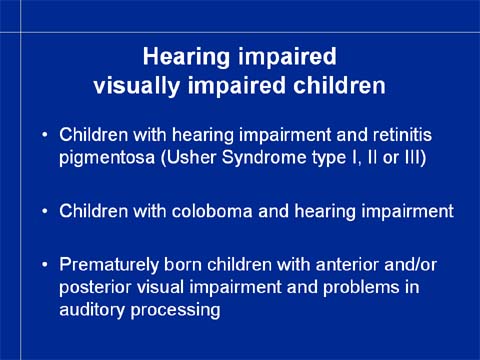
Among the hearing impaired children we have three different populations of children with visual impairment: 1. children with hearing impairment and retinitis pigmentosa (the Usher group), 2. children with hearing impairment and colobomas (due to rubella or different syndromes) and 3. children born prematurely and having anterior and/or posterior visual impairment and problems in central auditory processing due to early brain damage. Sometimes periventricular leukomalasia and scattered lesions in the brain cortex occurs in children born after normal pregnancy and without any obvious signs of the cause of the lesions.
Those nurses who serve schools for the deaf or classes for hearing impaired integrated children are advised to read about dual sensory impairment in the Part II of the Assessment Manual in my homepage.
Assessment of children with brain damage related visual impairment is also dealt with in the Part II of the Assessment Manual and briefly as the last group of multi-impaired children in this lecture. There has just been a WEBcast on CVI and it will be repeated in October - November 2004 (SKY-HI, VIISA, USU).
In the early intervention of infants with dual sensory impairment communication and interaction require intensive support and training of the parents from the very beginning so that bonding and interaction can develop. If the infant has colobomas and other closure defects in the midline, the disfiguration of the face before the first operations may be frightening to parents who have never seen such an infant. Pictures of other infants before and after the operations and videos like this short sequence may calm the emotional turmoil. Most parents need to watch videos of their own communication with the infant to really believe that the infant is interested in interaction and actually is quite skilful in it.
This video sequence depicts communication of a functionally deaf infant with bilateral colobomas. We see how tactile information is used to make the infant aware of something happening at the vocal cords and lips during communication (Tadoma for an infant).

Retinitis pigmentosa, slowly progressive degeneration of the retina due to apoptosis is more common among hearing impaired than among normally hearing children. Therefore it is advisable to screen hearing-impaired children for retinal dysfunction by using the CONE Adaptation test. Cone adaptation to lower, mesopic luminance levels becomes slower than normal quite early in the course of the degenerative changes. This feature is used in the CONE Adaptation test as the feature to be screened. The test comprises fifteen pieces of plastic, five white, five red and five blue.
First, the child is asked to sort the colors and put the small blocks to three piles, each color in its own pile. When a child has demonstrated that (s)he can do that, the same sorting is done in mesopic luminance. The illumination is arranged so that after the ceiling lights have been switched off, it takes about five seconds to start seeing the colors. All children start by picking the white chips because they glow in the dark. Since they are five, it takes about four to five seconds to pick them, after which the child starts to see the colors and sorts the red from the blue chips.
A child with delay in cone adaptation does not see the colors after five seconds and has to say (s)he does not know which is which. We have thus made an important functional diagnosis in less than ten seconds and without any costs.
In the test situation the surface under the the instructions on my homepage.
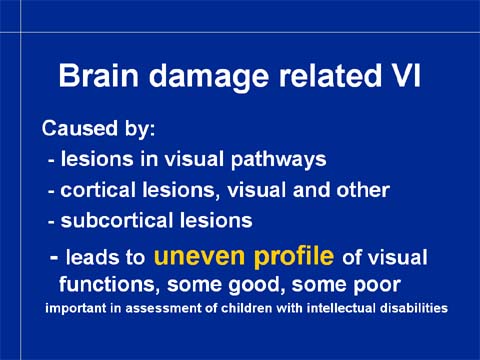
Brain damage related visual impairment or cerebral visual impairment, CVI, is caused by lesions in the long visual pathways, in the primary visual cortex or in the associative visual cortices. It is often combined with a whole host of impairments in other modalities and memory and in planning and executing activities. The diagnostic feature of brain damage to some visual functions is an uneven profile of visual functions, some functions are normal, other poor or do not exist at all. This is important to notice in children with intellectual disabilities because they may have specific losses of visual functions.
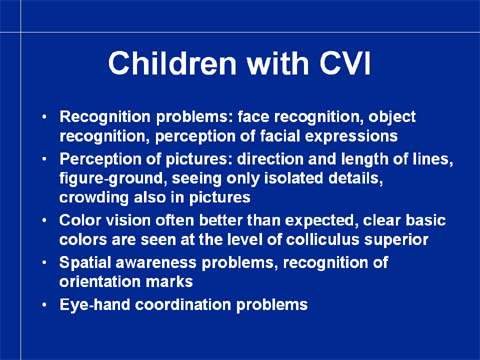
The common typical features of children with CVI are difficulties with form perception, recognition of faces, objects, landmarks and composite pictures. Difficulties can be also in perception and copying of the basic elements of images, the length and/or direction of lines, angles and even crosses. The difficulty can be at different levels of the chain of functions. Some children who make errors in copying do not perceive the difference between the correct and the wrong form but insist that they are exactly alike (inability to perceive visually). Other children can see the difference and say that their “hand does not do” what they want to draw, i.e. the problem is somewhere in the pathway from visual perception to motor planning and/or motor execution.
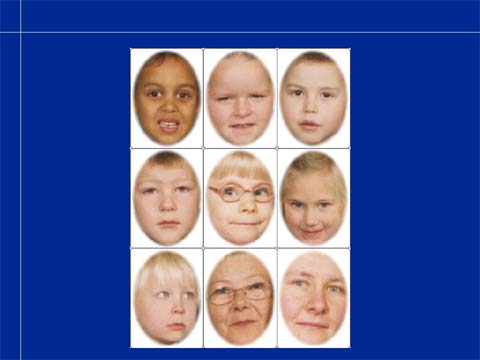
The girl in the middle of this slide is a typical example of children who have no face recognition, do not recognise even their family members. Since several people at the kindergarten did not want to believe that she had this problem, I made a specific test situation for her: in Photoshop, we made test cards of faces of her group of seven children so that only faces are visible. Of each card there are three copies. When the child came the next time for assessment, she was shown the cards and asked, who these people were. She did not know. She was told that they were at her kindergarten. This did not help. She was told that the pictures were pictures of the children in her own group. Then she said “the one with glasses must be me because I am the only one who has glasses”. Other children she couldn’t recognize.
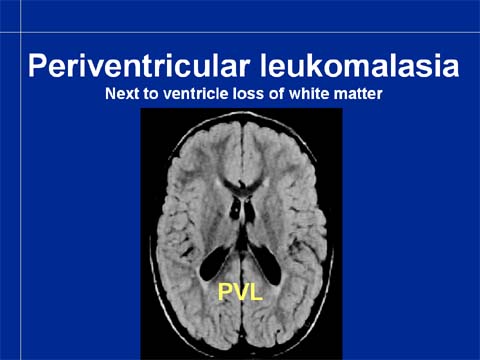
This girl has typical enlargement of the brain ventricles and loss of the periventricular white matter called periventricular leukomalasia, PVL.